女孩气管惊现神经纤维瘤 ,导致重度堵塞!医生智取“拦路虎”
2021-03-17 39健康网 39健康网
11岁女孩小朵(化名),呛咳后出现咳嗽、气促及胸痛,经检查发现其右主支气管内有一个肿物,并且右肺不张。
11岁女孩小朵(化名),呛咳后出现咳嗽、气促及胸痛,经检查发现其右主支气管内有一个肿物,并且右肺不张。由于肿物不断增大,引起重度气管梗塞,小朵的生命危在旦夕。经多学科会诊,广州市妇儿医疗中心胸外科李乐主任带领团队精准分离病变气管,为小朵成功切除肿物和右上肺叶,让她恢复顺畅呼吸。

手术在紧张进行中(医院供图)
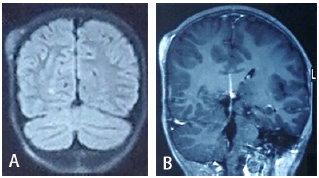
据介绍,小朵在入院后做了喉镜+纤维支气管镜探查,结果显示肿物将右主支气管完全阻塞,活检病理回报为纤维坏死组织。
此时,小朵只能向右侧卧,稍有活动或咳嗽便气喘不已。左肺全负荷工作勉强维持着通气,但右侧的肿物却虎视眈眈,随时可能阻断这一生命通道,解除气道梗阻已迫在眉睫。
当医生再次给予纤支镜治疗的时候,发现肿物较前增大,已接近气管隆突,并且由于其表面渗血而无法切除,手术成了挽救患儿生命的最后手段。
为了给患儿争取黄金救治时间,胸外科李乐主任和刘威主任第一时间召集麻醉科、呼吸科、PICU等多科专家进行MDT多学科讨论,商讨制定缜密的诊疗方案。
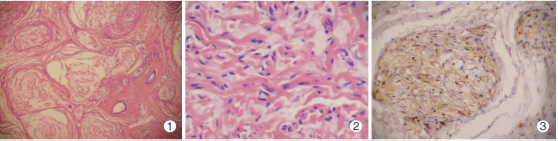
对于气道梗阻的患者,围术期的麻醉管理是手术成功的关键。而术中保持气道的通畅,防止术中肿物逆行脱落阻塞气管更是关键中的关键。麻醉科谭永红主任迅速制定个性化的麻醉方案,实施了该院首例儿童双腔支气管插管,保证了术中麻醉安全;呼吸科全程参与,通过支气管镜定位辅助手术顺利进行;病理科术中行快速冰冻病理分析,帮助判断肿物性质。
术中经纤支镜探查,肿物距气管隆突仅0.5cm。李乐主任在胸腔镜下避开隆突,精准分离气管病变,为了尽可能保留患儿右肺,采用右主支气管袖式切除+右肺上叶切除术。手术过程很顺利,术后小朵恢复良好,目前已经出院。
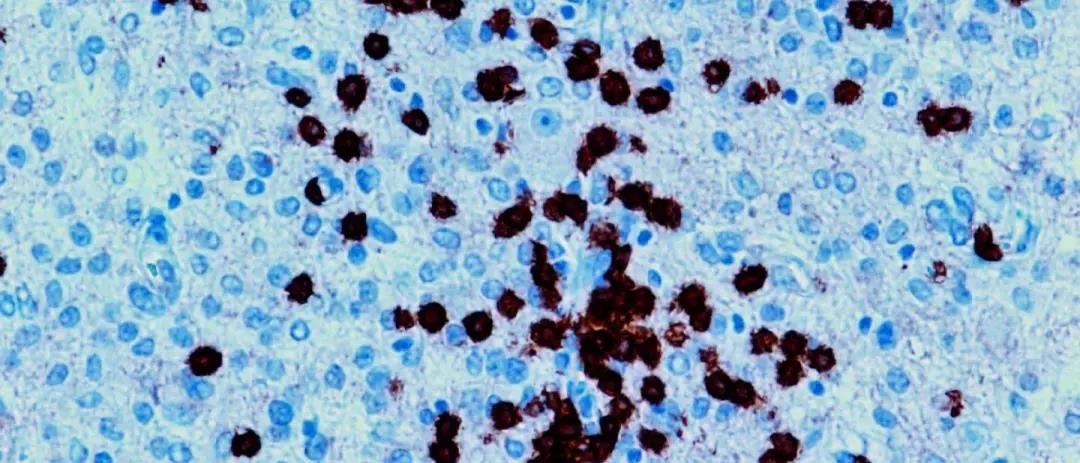
术后病理报告显示,小朵气管里的肿物是一种罕见的气管内神经纤维瘤。
据介绍,神经纤维瘤好发于躯干、四肢、头颈部、纵隔等,其患病率较低,约为3/10万, 发生于气管或支气管内者更极为罕见。
神经纤维瘤通常生长缓慢,病程较长,瘤体较小时症状较少;瘤体较大时可阻塞支气管引起呼吸困难、咳嗽等。由于其在气管的发生并不典型,容易被误诊为其他肿瘤,影像学诊断难度较大。而支气管镜检查能明确肿瘤部位和性质,较CT更为直观。治疗方面,外科手术疗效较好,条件允许时也可行纤支镜气道介入治疗。
虽然小朵目前已无大碍,但是术后仍然需要密切随访,提防神经纤维瘤复发。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#拦路虎#
53
哇塞
85
#纤维瘤#
75
#神经纤维#
88
了解
66
写的不错谢谢分享
105