Injury:掌侧锁定板治疗桡骨远端骨折的并发症
2014-05-14 佚名 丁香园
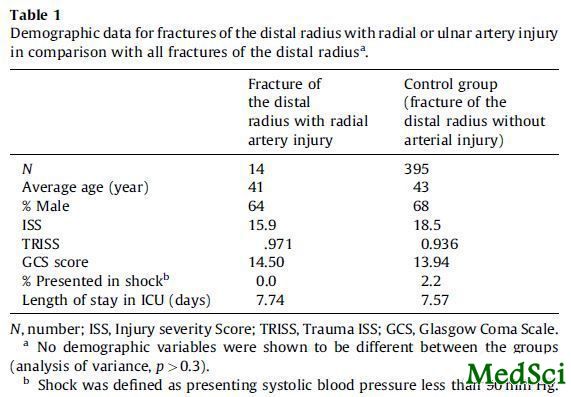
目前掌侧锁钉钢板是治疗桡骨远端骨折的主流。掌侧锁定板的优点包括生物力学稳定性好可以早期功能锻炼恢复腕关节功能;软组织并发症少。很多文献都报道了掌侧锁钉钢板治疗桡骨远端骨折成功率非常高。但该类钢板治疗桡骨远端骨折并发症发生率究竟有多高,英国创伤组织的回顾性研究对此给出了一个初步的答案。 该文回顾了从2009年1月至2010年12月206例应用掌侧锁定板治疗桡骨远端骨折的资料。随访36个月(24-4
目前掌侧锁钉钢板是治疗桡骨远端骨折的主流。掌侧锁定板的优点包括生物力学稳定性好可以早期功能锻炼恢复腕关节功能;软组织并发症少。很多文献都报道了掌侧锁钉钢板治疗桡骨远端骨折成功率非常高。但该类钢板治疗桡骨远端骨折并发症发生率究竟有多高,英国创伤组织的回顾性研究对此给出了一个初步的答案。
该文回顾了从2009年1月至2010年12月206例应用掌侧锁定板治疗桡骨远端骨折的资料。随访36个月(24-48个月)出现22例(9.7%)并发症,4例出现复杂区域疼痛综合征(CRPS),需要疼痛专科医师行进一步治疗。术后2周出现一例伤口浅表感染。1例患者术后1天出现畸形弯管综合征,急诊手术行腕管切开清除血肿减压。
7例(3.4%)病人出现肌腱问题,其中包括4例(19%)肌腱断裂。3例拇长伸肌腱(EPL)断裂和1例拇长屈肌断裂。3例(1.5%)患者出现骨折复位或移位问题,其中2例患者有较大桡骨茎突骨折块(图1)。这两例病人通过二次手术应用桡骨茎突钢板复位固定骨折块。4例(1.9%)病人因为内置物问题需要再次手术治疗。其中两例应用掌侧锁钉钢板和桡骨茎突钢板固定后出现持续性疼痛和腕关节功能受限。1例患者的一枚螺钉打入桡腕关节。另外1患者的一枚螺钉打入下尺桡关节。
该项回顾性研究是目前关于掌侧锁钉钢板并发症样本量最大的研究。在作者单位通过该研究的得出的数据,医生给患者解释各并发症发生几率:1/10的概率会出现并发症、1/30的概率出现肌腱问题。1/15的概率因为内固定物或者复位欠佳的问题需再次手术。 这样为患者提供了选择的量化依据。
原始出处:
Johnson NA1, Cutler L2, Dias JJ2, Ullah AS2, Wildin CJ2, Bhowal B2.Complications after volar locking plate fixation of distal radius fractures.Injury. 2014 Mar;45(3):528-33. doi: 10.1016/j.injury.2013.10.003. Epub 2013 Oct 14.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Injury#
94
#并发#
79
#桡骨远端骨折#
80
#桡骨#
88