导致血肌酐升高的原因,你了解多少?
2018-06-29 李青 天津市泰达医院 李青大夫
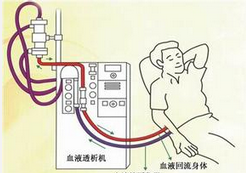
肌酐是肌肉的代谢废物,主要经肾脏排泄,正常值为男 54-106μmoI/L,女 44-97μmol/L。由于血肌酐每天产生的量相对恒定,排泄途径也相对单一,肾功能正常者,即使血肌酐产生增多,肾小球也会通过增加排泄来保持血肌酐水平稳定。因此,血肌酐水平可基本反映肾小球的滤过能力,即肾功能。血肌酐升高就提示肾功能减退,或者说肾功能衰竭,那么,导致血肌酐升高的原因都有哪些呢,一起来看一下吧!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肌酐#
61
#血肌酐#
79
好文献学习了
117
学习了
113
学习了受益匪浅
115