Crit Care Med:创伤后静脉血栓应得到重视
2012-08-21 MedSci MedSci原创
关于创伤后深静脉血栓栓塞发生率各个研究报导各不相同,有些报道甚至高达58%,但是目前临床上仍然认为创伤后不会出现深静脉血栓栓塞。影响深静脉血栓栓塞的危险因素包括:年龄,静脉栓塞病史,创伤类型,长时间制动等。由Greenfield等人提出的采用风险评估量表(RAP)量表来评估创伤后发生静脉血栓的风险在很多临床试验中被运用。该前瞻性观察性研究的目的是为了评估该量表是否能筛选出静脉血栓高危病人。并针对这
关于创伤后深静脉血栓栓塞发生率各个研究报导各不相同,有些报道甚至高达58%,但是目前临床上仍然认为创伤后不会出现深静脉血栓栓塞。
影响深静脉血栓栓塞的危险因素包括:年龄,静脉栓塞病史,创伤类型,长时间制动等。由Greenfield等人提出的采用风险评估量表(RAP)量表来评估创伤后发生静脉血栓的风险在很多临床试验中被运用。该前瞻性观察性研究的目的是为了评估该量表是否能筛选出静脉血栓高危病人。并针对这一高危人群预测影响深静脉血栓栓塞的独立危险因素。
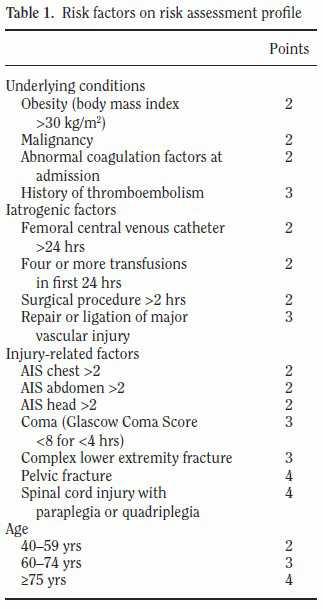
表1:风险评估量表
参与该研究的病人均为2009年11月至2012年1月期间收治入美国迈阿密大学瑞德创伤中心ICU病房,从中选取534位病人进行了风险评估量表评分,风险评估评分>10分的106位病人视为高危人群,在入院后24小时行常规静脉超声检查。此后每周进行超声检查。
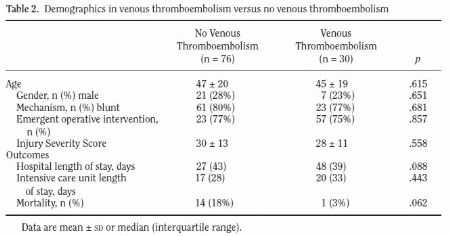
表2:发生静脉栓塞的病人和未发生病人人口特征比较
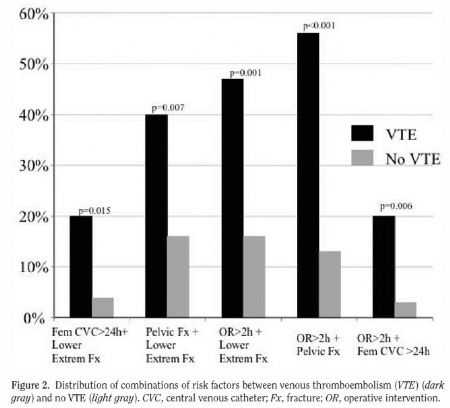
结果:106为高危病人中,静脉超声检测出20例 (19%)病人出现无症状深静脉血栓。其他途径检测出10例静脉血栓栓塞,包括6例有症状的深静脉血栓栓塞和4例肺栓塞,整体静脉血栓栓塞率为28%。出现静脉血栓栓塞的病人相对于没出现栓塞的病人,最常见的危险因素包括这些,经股静脉行中心静脉插置管(23% vs. 8%),手术干预>2h(77% vs. 46%),下肢复杂性骨折(53% vs. 32%)和骨盆骨折(70% vs. 47%),均有统计学差异 p <0 .05。发生静脉血栓栓塞的病人风险评估量表量表得分更高(19 ± 6 vs. 14 ± 4, p = .001). 风险评估量表量表得分(优势比1.14)和骨盆骨折后手术干预>2h(优势比5.75)是发生静脉血栓栓塞的独立危险因素。静脉血栓栓塞的发生率与是否是用抗凝治疗或使用不同的抗凝剂无关。
图1:发生静脉栓塞的病人和未发生病人危险因素分布比较。
文章作者得出结论:医疗机构将静脉血栓栓塞归为创伤后"从不出现的事件"这一做法值得商榷。从成本效益上来讲也许不适合对所有的创伤病人进行超声静脉血栓检测,但是可以考虑先用风险评估量表筛选出高危病人,对于这些病人,常规的超声检测和/或更积极地预防血栓方案也许能使他们受益。
原文链接:
Thorson CM, Ryan ML, Van Haren RM, Curia E, Barrera JM, Guarch GA, Busko AM, Namias N, Livingstone AS, Proctor KG.
Venous thromboembolism after trauma: A never event? Crit Care Med. 2012 Aug 10.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#静脉#
43
#静脉血#
67
#创伤#
51
#Med#
43