CVS 2016:王深明院长:作为血管外科医生,“开刀”技能不能丢!(附案例)
2016-08-13 MedSci MedSci原创
2016年8月11-14日,由中华医学会外科学分会和中华医学会外科学分会血管外科学组共同主办的2016年第13届全国血管外科学术会议在四川-成都隆重召开,梅斯医学作为特约媒体参与了此次盛会。来自中山大学附属第一医院血管外科,中山大学血管外科研究中心,中华医学会外科学分会血管外科学组组长王深明教授在开幕式上就“开放手术处理腹主动脉瘤腔内治疗后并发症”做了精彩报告。对此,梅斯医学小编进行了整理,与
2016年8月11-14日,由中华医学会外科学分会和中华医学会外科学分会血管外科学组共同主办的2016年第13届全国血管外科学术会议在四川-成都隆重召开,梅斯医学作为特约媒体参与了此次盛会。
来自中山大学附属第一医院血管外科,中山大学血管外科研究中心,中华医学会外科学分会血管外科学组组长王深明教授在开幕式上就“开放手术处理腹主动脉瘤腔内治疗后并发症”做了精彩报告。对此,梅斯医学小编进行了整理,与大家分享。

中山大学附属第一医院王深明院长
作为血管外科医生,“开刀”技能不能丢!
腹主动脉瘤越来越多地采用腔内治疗,开放手术所占比例越来越少,但腔内治疗失败后并发症不容忽视,仍需开放手术补救。OC(open conversion)是解决腔内修复术后并发症的重要方式。
腔内治疗并发症的常见原因
近期(术后30d内):支架无法输送到病变部位(入路狭窄、主动脉严重扭曲);支架无法正常打开(解剖因素,支架因素);定位失误(支架覆盖重要分支、支架植入夹层假腔等)
远期(术后30d后);持续内漏、瘤体增大、破裂、支架扭曲、移位、断裂、支架感染
文献回顾
在pubmed数据库中对endovascular repair & surgical conversion or conversion to surgery or open conversion进行检索,共检索到100多例的文献报道。
早期OC:20项研究,共20275例患者,早期OC272例,手术死亡率为10.7%
远期OC:34项研究,共26851例患者,远期OC715例,手术死亡率为9.9%
导致早期OC的主要因素:技术操作失败、支架定位失败,分体式支架衔接失败,重要内脏动脉被隔绝,I型内漏、III型内漏,短瘤颈,瘤体过大
导致早期OC的全身因素:高龄、低体重,COPD、吸烟、性别
导致远期OC的主要原因:瘤体持续增大,介入无法解决的I型、III型内漏,支架扭曲,夹层逆撕,Marfan综合征,植入多个支架,支架移植物感染,支架移植物移位,支架移植物结构故障,心脏--主动脉手术史
EUROSTAR(Eur J Vasc Endovasc Surg2004;27:128-137)共纳入114家医院,4613例腹主动脉瘤(AAA)患者,其中45例早期OC,早期OC30天死亡率13% vs 无OC2.3%(p<0.0001),3595例AAA患者完成随访32个月(3-60)共26例远期OC,远期OC总死亡率7.7% vs 无OC 7.4%
早期OC原因分析:
1,严重瘤颈成角:早期OC患者中严重瘤颈成角占23%,而无OC患者为11%
2,早期OC率:1996-1998年2.5%vs1999-2002年0.7%(p<0.0001)可能与支架设计、材料改进,以及操作技术水平提升有关
远期OC原因分析:
1,支架内血栓形成或狭窄:23%(p=0.02)
2,因支架移位:54%(p<0.0001)
3,因瘤体扩张:25%(p=0.017)
4,因瘤体破裂:23%(p<0.0001)
5,远期OC率:1996-1998年4.1%vs1999-2002年0.5%(p=0.056)
6,II型内漏:远期OC19%vs无OC9%(ns)
Life Registry (J Vasc Surg 2005 Jul;42(1):1-10)共纳入2664例AAA患者,其中68例(2.6%)早期OC,早期OC30天死亡率7.4%,随访1.2-4.4年(最长6.7年)共28例远期OC,死亡率为0。
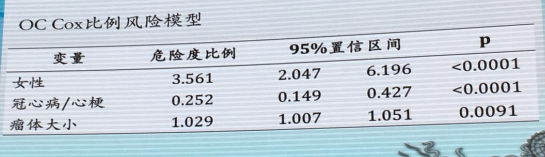
图:OC Cox比例风险模型
早期OC:女性患者8.9%vs男性患者2.7%(p<0.01),21例女性早期OC中19例归因于 动脉细小导致释放系统无法通过
远期OC:无性别差异
AURC(University Association for research in Vascular Surgery)(Eur J Vasc Endovasc Surg2009;38(4):429-434)共纳入8家发法国大学附属医院的1558例AAA患者,早期OC14例(0.9%),术后死亡率21%,远期OC20例(1.2%),术后死亡率15%。
Raidiol、吴子衡等(2014)回顾分析1994-2011年德国南纽伦堡医院行EVAR术1729例AAA患者资料,其中77例行远期OC,1994-2001远期OC手术率7.9%,2002-2011年远期OC手术率2.3%,围手术期死亡率5.2%,中位随访时间51月
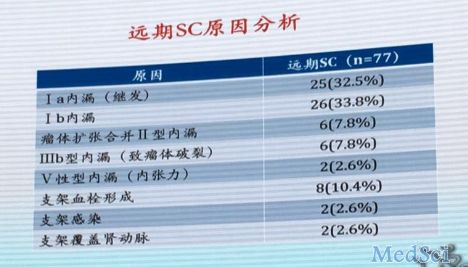
图:远期SC原因分析
总结
1,尽量避免腔内治疗并发症的发生是最重要的
2,术前严格把控腔内治疗指征、合理制定手术方案,选择合适的腔内移植物
3,术中注意精细操作、准确定位,出现问题时切记勉强施行,应随机应变,如有必要,适时转为开放手术
4,术后密切随访,及时发现问题、及时补救
5,腔内治疗一旦发生并发症,补救措施应当首选腔内治疗,但也不要“转牛角尖”,该“开放”时就“开放”,耐心寻找失败原因,有针对性的合理制定手术方案,可以是单纯开放手术或腔内治疗,也可以是杂交手术
全面考虑患者的病情和存在问题制定综合性治疗方案尽可能一次手术解决问题。
本文系梅斯医学(MedSci)整理,转载需授权!更多资讯请下载“梅斯医学APP”!扫一下二维码即可:

小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#CVS#
65
文章很好值得关注
89
学习到了
0
学习到了
87
值得学习
88
阅读了,不错
87
#血管外科#
60
#外科医生#
63
阅读了。
51
继续学习
50