JBJS:单节段腰椎后路融合BMP并不比自体髂骨更有优势
2013-07-26 JBJS dxy
自体髂骨移植植骨融合(ICBG)一直是脊柱融合术的金标准,但仍有接近2.8-39%不等的融合失败率。近十年,随着具有骨诱导活性的人工骨蛋白类rhBMP-2的开发,自体髂骨移植进行脊柱间植骨融合的地位受到了挑战。目前已有较多关于rhBMP-2应用效果的文献发表,多个多中心临床研究表明,rhBMP-2和ICBG在临床预后方面具有较多优势:手术时间,术中失血,住院周期,再手术率,恢复工作时间等均有所下降
自体髂骨移植植骨融合(ICBG)一直是脊柱融合术的金标准,但仍有接近2.8-39%不等的融合失败率。近十年,随着具有骨诱导活性的人工骨蛋白类rhBMP-2的开发,自体髂骨移植进行脊柱间植骨融合的地位受到了挑战。目前已有较多关于rhBMP-2应用效果的文献发表,多个多中心临床研究表明,rhBMP-2和ICBG在临床预后方面具有较多优势:手术时间,术中失血,住院周期,再手术率,恢复工作时间等均有所下降,而融合率则有所上升[2,7,8-10],而融合速度有所提高。但事实上,关于BMP在临床中是否有效仍存在持续争议,为进一步明确rhBMP-2和ICBG在单节段腰椎后路融合术(PLIF)中应用的优劣性,比利时的学者进行了单中心,前瞻性,随机对照研究,相关结论发表于近期出版的JBJS杂志上。
研究者设计该研究进行如下假设检验:第一,使用BMP组的患者因避免了髂骨供体部位的缺损而在临床上能获得较多收益;第二,在影像学检查上,使用BMP组的骨密度和骨小梁形成更少。
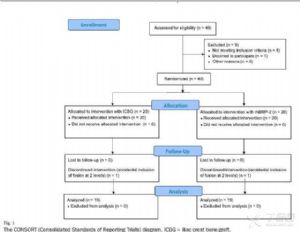
研究人群来自于2008年1月-2009年9月因腰椎脊柱前移,椎间盘蜕变保守治疗无效而接受单节段手术治疗的患者。共40例,按BMP组及ICBG组1:1比例划分,两组中各有1例患者因行两节段固定而除外(图1)。
术中使用器械包括:钛金属脊柱内固定系统(Medtronic),两个polyetheretherketone材质的融合器(Medtronic),rhBMP-2(InductOs)。
常规后路融合手术技术,2个融合器中填充各填充含2mg BMP的明胶海绵,同时在两个融合器前方各填充含2mg BMP的明胶海绵,每节段共计8mg BMP。
在术后3月,6月,12月及24月统计患者术后的功能指标,如VAS,ODI,SF-36 V2,并行CT检查,明确节段间融合,骨溶解,骨吸收等情况。
研究结果显示:
两组患者在大部分人口统计指标上无显著差异,仅在BMI上有显著差异(p=0.032)。BMP组手术时间(p=0.01),术中失血(p=0.08)等指标显著小于ICBG组。
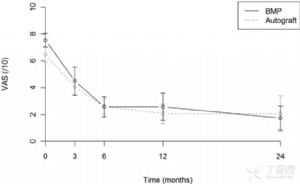
在术后功能评价指标方面,两组患者术后VAS,ODI,SF-36精神和身体评分均有显著改善(p<0.01),但组间比较无差异(p=0.987,p=0.577,p=0.536,p=0.278),如图2,3所示;
影像学CT检查提示,两组患者在3月,6月,12月,骨密度存在显著差异(p = 0.002, p = 0.024, and p = 0.014),如图4所示;BTB评分存在显著差异(p = 0.021, p = 0.004, and p = 0.014),如图5所示。
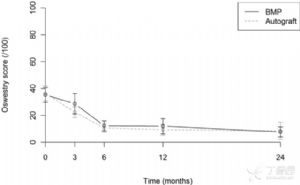
图2:研究组和对照组功能预后指标,均数标准差。图2-上,两组患者术前,术后3月,6月,12月及24月VAS评分;图2-下,两组患者术前,术后3月,6月,12月及24月ODI评分

图3:研究组和对照组功能预后指标,均数标准差。图3-a,两组患者术前,术后3月,6月,12月及24月SF-36身体功能评分;图2-b,两组患者术前,术后3月,6月,12月及24月SF-36精神评分

图4:研究组和对照组术后不同时间点骨密度对比(p = 0.002, p = 0.024, p = 0.014)。
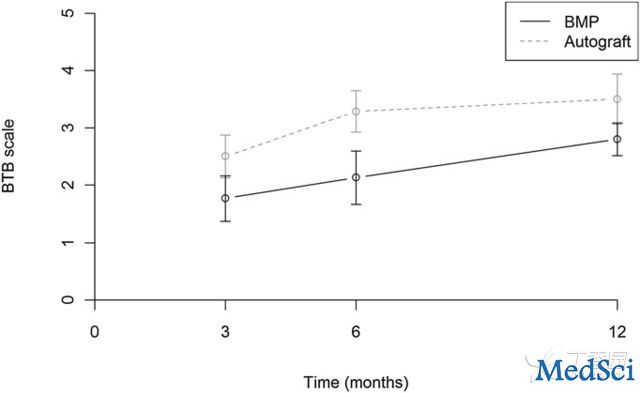
图5:研究组和对照组术后不同时间点BTB对比(p = 0.021, p = 0.004,p = 0.014)。
不良事件:BMP组有1/19例患者出现一过性神经根痛,所有患者在3月时均出现终板吸收(图6所示),而有7/19例患者出现骨吸收,2/19例患者出现空洞形成(图7),7/19例患者出现异位骨化。而ICBG组上述不良事件发生率为0,但ICBG组供体髂骨区域有2例患者在术后3月存在疼痛,术后1年所有患者均无不适感觉。

图6:术后不良事件实例。图6-a,接受BMP治疗患者融合节段的矢状位CT重建,提示在3个月时有椎体终板的吸收,在6月时椎体间骨形成,在12月时有异位骨化形成,在24月时,异位骨化广泛发展。图6-b,同一例患者,术后24月轴位CT,提示在椎管内广泛异位骨化形成,并向脊柱上下关节突延伸。

图7:使用BMP融合的患者CT扫描显示术后3月,终板后部吸收,术后12月,在融合器后方有异位骨化及骨空洞形成。但患者无明显神经根刺激症状。
研究者在讨论中分析:
1.研究的第一个假设不成立,尽管ICBG显著增加了手术时间和术中失血,但并未显著改变患者术后的功能预后。第二个假设成立,BMP组在骨密度和骨小梁形成方面要显著低于ICBG组,这提示BMP的使用可能从某种程度上减慢了骨形成的速度。
2.本研究观察到仅BMP组出现短暂的神经根刺激症状,结合既往文献报道,使用BMP者神经根刺激的发生率约在7-14%之间,而ICBG后路融合术的神经根刺激发生率仅2-7%,研究者认为神经根刺激可能是机械压迫和化学刺激双重作用结果。
3.在本研究中,BMP组患者出现了骨溶解,空洞,异位骨化形成,而对照组无患者出现上述情况,提示骨溶解是因为BMP诱导,而非早先报道的终板变化导致。
研究者最后总结认为:rhBMP-2在后路植骨融合中的短期作用(1年内)和ICBG相当,在融合率方面无显著差异,但BMP组术后相关的不良事件如骨溶解,终板骨吸收,异位骨化等发生率更高。

Michielsen J, Sys J, Rigaux A, Bertrand C.The effect of recombinant human bone morphogenetic protein-2 in single-level posterior lumbar interbody arthrodesis.J Bone Joint Surg Am. 2013 May 15;95(10):873-80. doi: 10.2106/JBJS.L.00137.PMID:23677353
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BMP#
70
#腰椎#
68
#融合#
51
#JBJS#
47