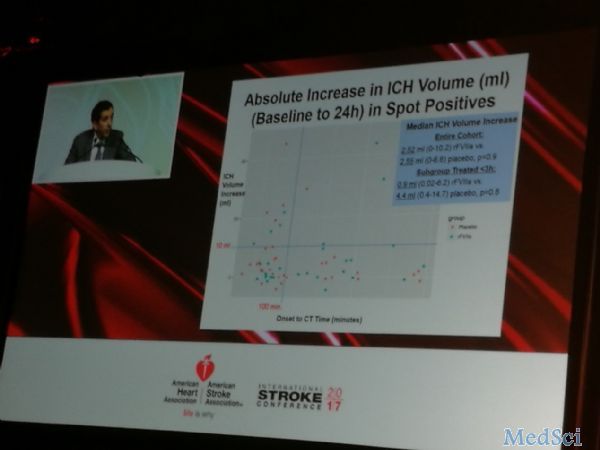
2017 ISC:脑出血到底有没有止血药?
2017-03-17 董漪 壹生
急性缺血性卒中有阿替普酶,而急性脑出血至今尚没有可以急性应对的药物,可减少致残率和死亡率。因此本研究期待通过寻找最佳合适治疗人群,应用凝血因子VII减少再出血体积,以期待治疗脑出血的治疗之药。美国每年大约79500例脑出血患者中,约10%的患者使用了未经证实的药物、死亡率较高。前期研究发现约40%的脑出血患者可能出现出血加重,而目前循证的治疗土建仅仅血压控制、支持治疗及在特殊病例中的手术治疗。FA
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#止血药#
96
感谢分享,长见识了
111
感谢分享,长见识了
105
#止血#
83
#ISC#
83
谢谢分享
92
好好学习,涨知识
105