Cardiovasc Diabetol:心脏磁共振组织追踪评价2型糖尿病患者主动脉瓣关闭不全程度对左心室应变的累加效应
2022-03-16 从医路漫漫 MedSci原创
2型糖尿病(T2 DM)及其相关心血管疾病在发病率和死亡率方面造成越来越大的负担。
背景:2型糖尿病(T2 DM)及其相关心血管疾病在发病率和死亡率方面造成越来越大的负担。T2 DM的特征是胰岛素利用不足或无效,导致慢性高血糖。如果糖尿病导致左心室(LV)重构,并增加退行性主动脉瓣疾病的风险,就会发生主动脉瓣反流(AR)。这种现象会导致左心室负荷和一系列心脏损伤。除了经常被研究的危险因素外,T2 DM与AR的高风险相关,即使大多数患者没有症状并经常被忽视,它也是未来的一个增量挑战。伴有AR的T2 DM患者心脏结构、功能和张力的变化尚不完全清楚,难以量化。以前的研究已经调查了T2 DM或AR作为独立实体对心脏结构和功能的独立影响。此外,基于心脏应变的综合效应还没有得到充分的评估。因此,在不良事件发生前调查伴有AR的T2 DM患者的心功能障碍对于降低心血管风险和改善预后具有重要意义。
心脏磁共振(CMR)组织跟踪技术基于标准稳态自由进动电影图像的后处理,已成为一种被广泛接受的量化糖尿病相关心脏变形功能障碍的成像工具。CMR可以提供有关亚临床条件下左室应变的独特信息,并在左心室射血分数(LVEF)或内径变化之前敏感地识别结构和功能变化。此外,它还可以定量和数字化地识别早期信号,用于心肌损伤的诊断和治疗。因此,本研究旨在比较左室结构、功能和应变的特点,探讨AR是否加重左室变形功能障碍,并确定影响T2 DM合并AR和不伴AR的T2 DM患者LV整体峰值应变(PS)的独立因素。
方法:共215例T2 DM患者和83例年龄、性别匹配的健康体检者接受心脏磁共振检查。根据超声心动图将2型糖尿病合并AR患者分为3组:轻度AR组28例,中度AR组21例,重度AR组17例。比较LV功能和整体应变参数,并进行多因素分析以确定LV PS的独立指标。结果:合并AR的T2 DM患者的左心室整体PS、收缩应变率峰值(PSSR)和舒张期应变率峰值(PDSR)在三个方向上均低于无AR组和非T2 DM对照组。无AR患者的三个方向的PS(径向和纵向)和PDSR低于正常对照组,PSSR(径向和纵向)高于正常对照组。此外,返流程度是影响左心室整体径向、周向和纵向PS的独立因素。
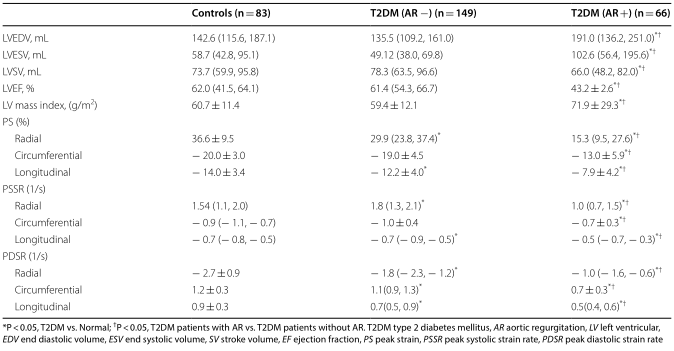
表1 2型糖尿病伴/不伴AR患者与正常对照组CMR结果比较
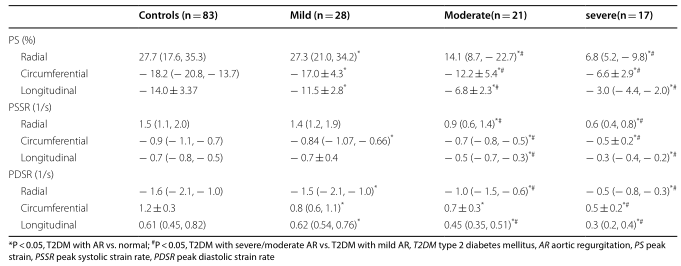
表2 2型糖尿病轻、中、重度反流患者与正常对照组左心室应变的比较
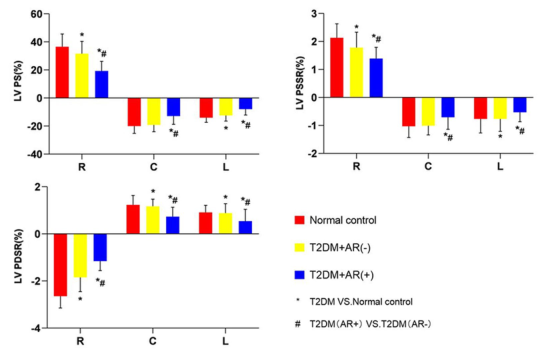
图1对照组、T2 DM(AR-)和T2 DM(AR+)在LV PS(%)、PSSR(1/s)、PDSR(1/s)中的CMR推导的LV应变参数。#有AR的T2 DM患者与无AR的T2 DM患者#P<0.05。T2 DM,2型糖尿病;AR,主动脉瓣关闭不全;LV,左心室;PS,峰值应变;PSSR,峰值收缩应变率;PDSR,峰值舒张期应变率
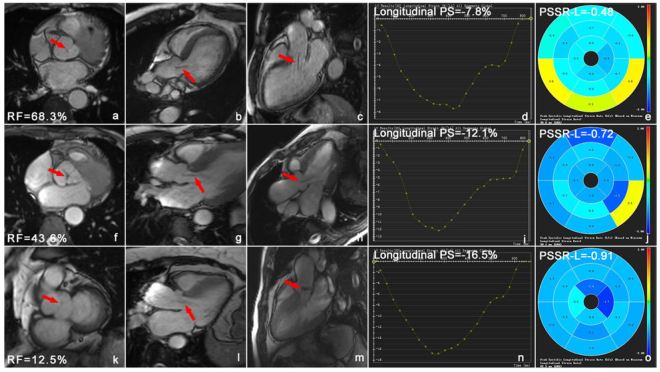
图2 有轻度、中度和重度反流的T2 DM患者的心脏电影图像和左心室纵向应变的三维伪彩色图像。A-c-T2 DM伴重度主动脉瓣关闭不全患者,男,59岁,左室短轴(A)、四腔(B)、双腔(C),Rf=68.3%,f-h,T2 DM伴中度主动脉瓣关闭不全,女,52岁,左室短轴(F),四腔(G),双腔(H)电影序列图像显示中度主动脉瓣反流(红色箭头),Rf=43.6%;2型糖尿病合并轻度主动脉瓣关闭不全患者,男性,58岁,左室短轴(K)、四腔(L)、双腔(M),Rf=12.5%。D、i、n和e、j、o是左心室PS和PSSR的纵向三维伪彩图。电影序列图像显示从主动脉到左心室的黑色返流信号(红色箭头)。2型糖尿病、RF返流分数、PS峰值应变率、PSSR收缩应变率
结论:AR可加重T2 DM患者的左心室僵硬,导致左心室应变和功能降低。T2 DM和AR患者的反流程度和性别与LV整体PS独立相关。
原文出处:Shen LT, Jiang L, Zhu YW,et al.Additive effect of aortic regurgitation degree on left ventricular strain in patients with type 2 diabetes mellitus evaluated via cardiac magnetic resonance tissue tracking.Cardiovasc Diabetol 2022 Mar 11;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BET#
69
#ASC#
73
#DIA#
68
#主动脉瓣#
88
#磁共振#
73
#2型糖尿病患者#
83
#心脏磁共振#
69
#左心室#
0
#主动脉#
69
#评价#
72