JNNP:孤立性脊髓炎患者后期转为多发性硬化的早期相关因素
2021-03-18 MedSci原创 MedSci原创
多发性硬化(MS)的诊断标准已经演变为有助于在疾病早期诊断MS。因此,许多以前被认为患有“横断性脊髓炎”或“临床孤立综合征”的患者,现在可以在第一次临床
多发性硬化(MS)的诊断标准已经演变为有助于在疾病早期诊断MS。因此,许多以前被认为患有“横断性脊髓炎”或“临床孤立综合征”的患者,现在可以在第一次临床事件时诊断为MS。此外,对其他特定原因的诊断也有了进展,原因包括高分辨率MRI,发现抗体介导疾病(如视神经脊髓炎频谱障碍)的敏感和特异性血清学检查;以及更好地识别其他炎症和非炎症性疾病急性至亚急性脊髓病(如自发性脊髓梗死和神经瘤)的原因。最近的研究表明,目前有大量脊髓病患者可以诊断为特定的病因,然而,与“横断性脊髓炎”或“特发性横断性脊髓炎”的非特异性标签不同。但是,仍有一类患者存在孤立性脊髓炎。这些患者中的一些可能在以后的几年中有患MS的风险,这是从预测、监测和开始治疗的角度考虑的一个重要因素。本研究的目的是确定早期因素预测后转为MS的患者的孤立性脊髓炎。

回顾性了2010年1月至2018年3月期间,作为新患者或回诊患者的病历。主治医师在每一例中指定的临床诊断记录下来,然后由两名神经科医生(OCM和CAP)中的一名或两名同时具有脊髓病诊断和管理专业知识的两名神经科医师确认。这种严格的诊断验证符合小组之前描述的方法,重点是仔细区分脊髓病的炎症和非炎症原因,然后描述特定的潜在病因(如神经瘤病,可能的话,中枢神经系统感染或系统性风湿性疾病。根据临床实践,在临床就诊的个别患者中,具体的病因试验不同,但通常包括对与脊髓炎相关的风湿性疾病(系统性红斑狼疮、Sjögren综合征、Behçet病、混合结缔组织疾病)的实验室筛查,抗体相关疾病(AQP-4-IgG)和近年来髓鞘少突胶质细胞糖蛋白IgG(MOG IgG)),以及脊髓炎的传染原因(莱姆病、梅毒、HIV、疱疹病毒、肠病毒、地理和季节相关的黄病毒)。在提示性临床和影像学表现的患者中,本组发表的工作一致,6例患者认为结节病相关脊髓炎,并在显示的情况下进行全身成像(CT胸部和/或PET体)和组织活检进行调查。在说明的地方,研究了其他罕见的脊髓炎的病因(如慢性淋巴细胞炎症伴桥旁血管周围增强对类固醇或副肿瘤疾病的反应)。
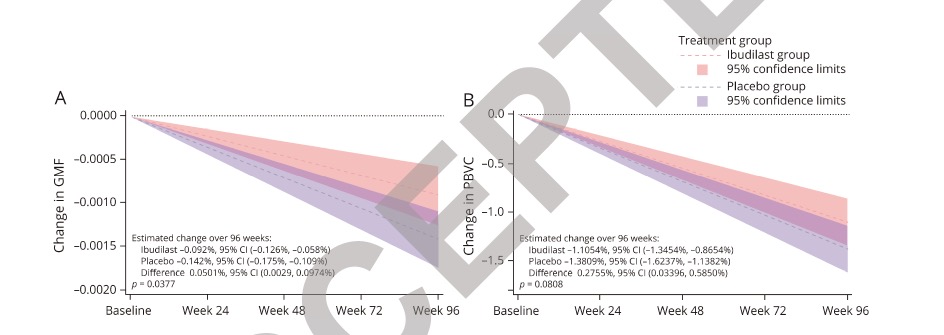
100例患者,平均随访4.3年。在77例短节段脊髓炎(MRI上最长病变范围<3个椎体)患者中,25例(32%)发生MS,而在23例纵行广泛性脊髓炎患者中,0例(0%)发生MS(p=0.002)。在短节段脊髓炎患者中,使用多变量logistic回归分析确定的高度预测转为MS的因素包括脑脊液(CSF)限制性寡克隆带(OCB)(OR(OR)9.2,95%CI 2.1至41.0,p=0.004),年龄较小(OR 1.1/年,95%CI 1.0至1.1,p=0.04)和更长时间的随访(或更长时间每年1.3,95%可信区间1.0至1.6,p=0.04)。脊髓炎发作后平均2.8年转为多发性硬化。

短节段MRI脊髓病变、脑脊液局限性OCB、年龄小、随访时间长是孤立性脊髓炎患者转为MS的预测因素。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#多发性#
104
#脊髓炎#
98
#相关因素#
70
#孤立性#
72