Nat Commun:肺动脉高压的内皮细胞中activin-A/BMPR2通路被异常激活
2021-03-26 xiaozeng MedSci原创
肺动脉高压(PAH)是一种罕见的进行性的致命疾病,全球每100万人中约有15至50例。
肺动脉高压(PAH)是一种罕见的进行性的致命疾病,全球每100万人中约有15至50例。持续性的肺动脉高压会导致右心室肥大,并最终导致右心衰竭。
由于目前该疾病的治疗选择仍有限,因此开发新的治疗策略显得迫在眉睫。PAH的病理特征在于病理性肺动脉的功能重塑。然而其详细的分子机制仍有待阐明。既往研究显示,内皮细胞(EC)功能障碍,如血管生成失调、细胞增殖和凋亡的非正常增加等,已被证实为该疾病的主要原因之一。
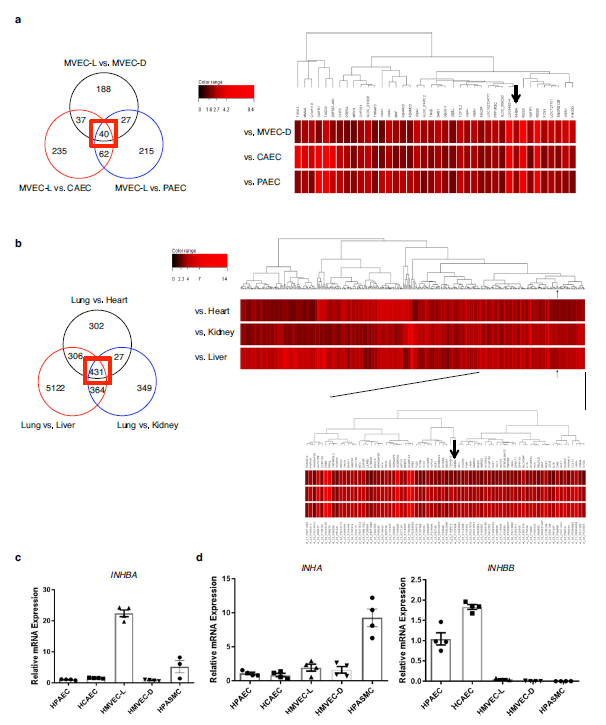
该研究描述了在血管性高血压中内皮血管分泌的作用。通过分析肺毛细血管内皮细胞中高表达的基因,研究人员发现,inhibin-β-A(抑制素-β-A)是由肺毛细血管产生的血管分泌因子。内皮细胞inhibin-β-A的过量产生能够以自分泌方式行使activin-A(激活素-A)的功能并损害了内皮功能。机制研究显示,activin-A能够诱导BMPR2(2型骨形态发生蛋白受体)的内化并靶向溶酶体途径的降解作用,并最终导致内皮细胞信号的缺乏。
抑制素-β-A为肺毛细血管的高表达基因
值得注意的是,相比于从正常对照的肺部分离内皮细胞,从特发性肺动脉高压患者的肺部分离出的内皮细胞显示出了更高的inhibin-β-A表达水平并产生更多的activin-A。当小鼠内皮细胞的activin-A/BMPR2通路被过度驱动时,会加剧缺氧诱导的肺动脉高压,而条件性敲除内皮细胞中的inhibin-β-A则能够阻止肺动脉高压的发展。
总而言之,该研究结果揭示,内皮细胞中activin-A/BMPR2通路的失调对于肺动脉高压的发展起着关键作用,因此inhibin-β-A/activin-A可能是该疾病的潜在药物治疗靶标。
原始出处:
Ryanto, G.R.T., Ikeda, K., Miyagawa, K. et al. An endothelial activin A-bone morphogenetic protein receptor type 2 link is overdriven in pulmonary hypertension. Nat Commun 12, 1720 (19 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#COMMUN#
53
#BMP#
81
#Nat#
57
#动脉高压#
57
学到了很多东西谢谢老师
92
学到了很多东西谢谢老师
101
学到了很多谢谢老师
96
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
64