Lancet:生物可吸收血管支架在冠状动脉疾病患者中应用1年的效果
2016-01-28 MedSci MedSci原创
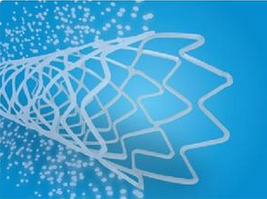
与金属药物洗脱支架相比,生物可吸收血管支架(BVS)具有改善经皮冠状动脉介入长期结果的可能性。这些设备是否在植入后第一年内和药物洗脱支架一样是安全和有效的并不为人所知。原始出处:Gregg W Stone,Runlin Gao,Takeshi Kimura,et al.1-year outcomes with the Absorb bioresorbable scaffold in patient
与金属药物洗脱支架相比,生物可吸收血管支架(BVS)具有改善经皮冠状动脉介入长期结果的可能性。这些设备是否在植入后第一年内和药物洗脱支架一样是安全和有效的并不为人所知。
研究人员做了一项四项随机试验的患者级,汇集荟萃分析,其中3389例稳定性冠状动脉疾病或稳定的急性冠脉综合征患者被招募于北美,欧洲,以及亚太地区的301个学术和医疗中心。这些患者被随机分配接受依维莫司洗脱吸收BVS(n=2164)或Xience钴铬依维莫司洗脱支架(CoCr-EES;n=1225)。主要终点是以患者为导向的复合终点1年相对率(全因死亡,所有心肌梗死或全部血运重建)和设备的靶病变失败(心源性死亡,靶血管相关心肌梗死或缺血导致的靶病变血运重建)。所有分析都是通过意向性治疗获得的。
对于BVS和CoCr-EES,以患者为导向的复合终点的1年相对速率总的治疗效果没有差异(相对风险[RR] 1.09 [0.89-1.34],p= 0.38)。同样,以设备为导向的复合终点事件的1年相对速在两组之间没有差异(RR 1.22 [95%CI 0.91-1.64],P=0.17)。与CoCr-EES相比,使用BVS的患者靶血管相关的心肌梗死增加(RR 1.45 [95%CI 1.02-2.07],p=0.04),部分原因是由于使用BVS的患者在围手术期心肌梗死和设备血栓形成(RR 2.09 [0.92-4.75],P=0.08)。全因死亡率和心源性死亡,所有心肌梗死,缺血导致的靶病变血运重建,所有血运重建的相对概率在BVS和CoCr-EES之间没有差异。当两个随访时间不到1年的随机试验被包含在内时,对于基线失衡进行多变量校正后的结果是相似的,并且在大多数亚组和敏感性分析中是一致的。
在这个荟萃分析中,与CoCr-EES相比,在1年的随访时,BVS并没有导致以患者为导向和以设备为导向的不良事件发生的概率不同。
原始出处:
Gregg W Stone,Runlin Gao,Takeshi Kimura,et al.1-year outcomes with the Absorb bioresorbable scaffold in patients with coronary artery disease,Lancet,2016.1.26
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#可吸收#
70
#生物可吸收#
55
#Lancet#
109
#疾病患者#
91
#冠状动脉疾病#
90