Cell Discovery:上海巴斯德所揭示迷走神经调控急性肺部感染免疫的新机理
2017-04-19 佚名 上海巴斯德研究所
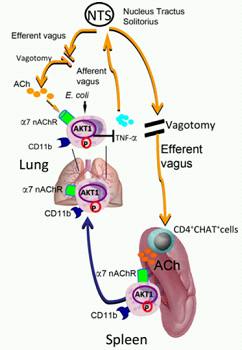
4 月 11 日,国际学术期刊《细胞发现》(Cell Discovery)在线发表了中国科学院上海巴斯德研究所苏枭研究组最新研究成果《迷走神经 - 脾脏协同调控急性肺部感染损伤的分子机制》(Signals of vagal circuits engaging with AKT1 in α7 nAChR+CD11b+ cells lessen E. coli or LPS‐induced acute
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cell#
53
#Dis#
59
#cover#
72
#CEL#
0
感谢分享一下!!
94
继续学习。
81
#肺部感染#
162
#ISC#
66