ASCO2017:NKTR-214促进患者免疫细胞增殖以及PD-1表达
2017-05-20 鱼会飞 艾兰博曼医学网
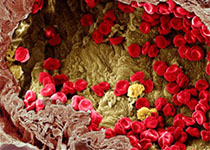
新型IL-2细胞因子免疫激动剂(NKTR-214)是CD122依赖型的激动剂,可以通过异源二聚体IL-2受体途径(IL-2Rβɣ)提供持续的信号转导,还可以在肿瘤卫环境中通过调节性T细胞刺激CD8+ T细胞和NK细胞的增殖。本研究在局部晚期或转移性实体瘤患者中对经过NKTR-214治疗后的肿瘤微环境的免疫变化进行了评估。
新型IL-2细胞因子免疫激动剂(NKTR-214)是CD122依赖型的激动剂,可以通过异源二聚体IL-2受体途径(IL-2Rβɣ)提供持续的信号转导,还可以在肿瘤卫环境中通过调节性T细胞刺激CD8+ T细胞和NK细胞的增殖。本研究在局部晚期或转移性实体瘤患者中对经过NKTR-214治疗后的肿瘤微环境的免疫变化进行了评估。
研究采用以下方法,对IV期的门诊的肿瘤患者进行q2w(两周一次)或q3w(三周一次)的NKTR-214治疗。采集血液和肿瘤组织样品,用流式细胞术、免疫组化(IHC)、T细胞克隆、基因表达分析等方法进行免疫活性的测定。
在三周一次经NKTR-214治疗的26例患者中,接受的治疗剂量分别为4例0.003mg / kg、9例0.006 mg / kg、6例0.009 mg / kg和1例0.012 mg/kg。研究结果表明,二周一次治疗的患者有6例接受0.006 mg/kg的NKTR-214治疗。最常见的Gr1-2 TRAEs为疲劳(73%)、瘙痒(65%)、食欲不振(46%)。1例患者在最高剂量下出现Gr3昏厥和低血压反应,并以较低剂量继续治疗。没有与药物相关的AEs导致研究停止。没有观察到与免疫相关的AE或者毛细血管渗透综合征。6例(23%)的患者肿瘤发生了10-30%的缩小。3例没有接受过免疫治疗的患者在结束NKTR-214治疗后,在接受抗PD-1治疗后肿瘤明显消退。所有患者的血液样品检测治疗8天后新增殖(Ki67 +)T和NK细胞增加。流式细胞术和/或IHC显示肿瘤微环境中肿瘤CD8 + T和NK细胞的基线增加高达10倍,Treg的变化最小。PD-1表达在TIL中增加2倍。 肿瘤组织的基因表达分析显示几种免疫检查点基因、细胞毒性标志物(IFNg, PRF1, and GZMB)以及T细胞克隆性都有所增加。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NKT#
79
#ASC#
40
#NKTR-214#
55
#细胞增殖#
62
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
92
学习并分享了
102
学习有益,谢谢分享
84
非常好的文章,学习了,很受益
99
学习了,感谢分享!
74
又发现新的标志物,对肿瘤领域又是一个进步
56