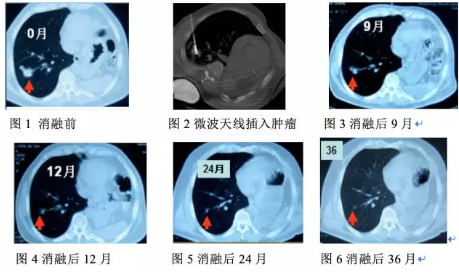
肺癌微波消融治疗经验分享
2018-04-28 撰写 | 叶欣(山东省立医院 )编辑 | 狄迪 中国医学论坛报今日肿瘤
在世界范围内,肺癌的发病率和死亡率居癌症之首,全球每年发病约250万例,每年有超过160万人死于肺癌。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#经验分享#
75
新技术.值得推广学习.
106
#消融#
74
#消融治疗#
74
学习了.谢谢分享
117
不错的文章值得拥有
101
不错的文章值得推荐
115
^_^^_^^_^
129