Neurocrit Care:脑出血6h内很大中线移位>4mm者预后不良
2018-08-04 杨中华 脑血管病及重症文献导读
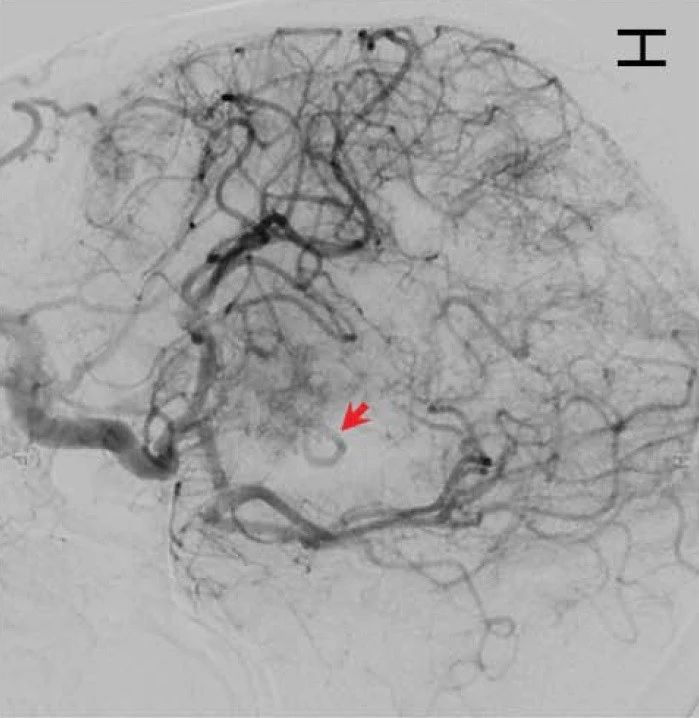
脑出血(ICH)是一种具有摧毁性的事件,与高死亡率和高残疾率有关。死亡率从7天时的35%到1年时的59%,不足40%的患者恢复功能独立。基线血肿体积联合其他因素,比如年龄、基线CT脑室内出血、入院GCS评分,可以预测自发性ICH的临床预后。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ROC#
69
学习了,谢谢分享
106
#预后不良#
58
好文章学习了
87
学习了很有用不错
67
阅
89
谢谢分享,学习了
77