JAMA Cardiol:早绝经提示女性动脉粥样硬化性心血管疾病风险升高
2021-09-22 Nebula MedSci原创
早绝经与女性动脉粥样硬化性心血管疾病风险呈正相关
当代实践指南建议,使用合并队列方程 (PCE) 来预测 10 年动脉粥样硬化性心血管疾病 (ASCVD) 的风险。为了个性化患者与临床医生对 ASCVD 风险的讨论,最新的 ACC/AHA 指南将早绝经确认为 40 岁以下女性的 ASCVD 风险增加因素。
但是,除了糖尿病、高脂血症、高血压和肥胖等传统风险因素外,目前尚不清楚早绝经对 ASCVD 的风险预测的影响大小。该队列研究评估了在 PCE 中加入早绝经状态对女性 ASCVD 的风险预测的影响。
研究人员汇集了来自 7 个美国人口队列的 40-79 岁的绝经后女性(黑人和白人)的数据,排除有 ASCVD 病史的女性。根据 2019 年 ACC/AHA 指南将早绝经定义为 40 岁以前绝经。ASCVD 被定义为致死性或非致死性的冠心病或卒中。

有无早绝经女性的基础特征
共纳入了 5466 位黑人女性和 10584 位白人女性。黑人女性的年龄更大,高血压、肥胖症和糖尿病的患病率更高。与白人女性(9.8%)相比,黑人女性早绝经更普遍 (17.4%)。此外,独立于传统危险因素,早绝经与 ASCVD 显著相关,在黑人和白人女性中的风险比分别是 1.24 (95% CI, 1.03-1.49) 和 1.28 (95% CI, 1.13-1.45)。
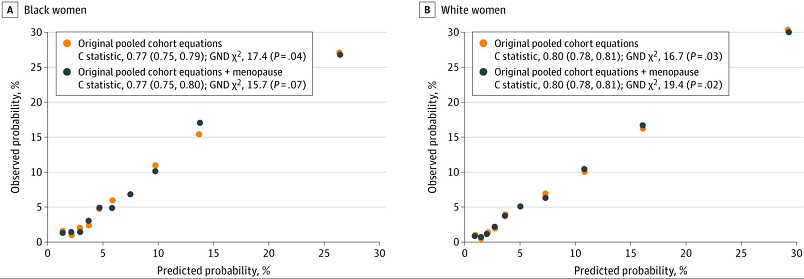
有无早绝经女性原始汇集队列方程的模型表现
PCE 对两组均表现出良好的区分和校准表现。但是,将早绝经加入 PCE 后,ASCVD 的风险预测没有增加额外的益处,黑人和白人女性的分类 NRI 值分别为 0.0007(P=0.91)和 0.003(P=0.37)。在敏感性分析中,对于自然绝经的女性、手术绝经的女性以及 40-54 岁的女性,在模型性能方面也观察到了类似的结果。
综上,该研究结果与既往研究一致,提示早绝经与 ASCVD 风险呈正相关。该研究结果还支持早绝经是 ASCVD 的风险增强因素。但是,将早绝经添加到 PCE 中并没有显著改善 ASCVD 风险预测。
原始出处:
Freaney PM, Ning H, Carnethon M, et al. Premature Menopause and 10-Year Risk Prediction of Atherosclerotic Cardiovascular Disease. JAMA Cardiol. Published online September 15, 2021. doi:10.1001/jamacardio.2021.3490
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
118
#Cardiol#
104
#粥样硬化性#
126
学习
117
#绝经#
113
#动脉粥样硬化性心血管疾病#
116
#疾病风险#
105
#硬化性#
120
#血管疾病#
103
妇科药物绝经的患者要提高警惕了
133