PLOS Biology:清华北大合作揭示一种新的细胞死亡途径,为中风治疗带来新靶点
2021-05-06 “E药世界”公众号 “E药世界”公众号
法尼基焦磷酸(Farnesyl Pyrophosphate,简称FPP),是存在于甲羟戊酸途径中的一个中间产物,用于在生物体内生物合成萜、类萜与甾醇,有助于蛋白质合成、能量产生和细胞膜构建等等,因此通

法尼基焦磷酸(Farnesyl Pyrophosphate,简称FPP),是存在于甲羟戊酸途径中的一个中间产物,用于在生物体内生物合成萜、类萜与甾醇,有助于蛋白质合成、能量产生和细胞膜构建等等,因此通常被认为是无害的分子。
2021年4月26日,清华大学生命学院刘万里、张永辉、北京大学神经科学研究所张勇作为共同通讯作者,在 PLOS Biology 期刊发表了题为:Farnesyl pyrophosphate is a new danger signal inducing acute cell death 的研究论文。
该研究发现,正常细胞代谢中的重要中间体法尼基焦磷酸(FPP)也是引发细胞死亡的诱因,该发现可能有助于更好地了解中风引起的损伤,并为开发中风治疗药物提供了有潜力的靶点。
法尼基焦磷酸(FPP)通常以很低的浓度存在于微环境中,不会触发细胞死亡,但可能会在缺血性中风期间发生变化,因为已知甲羟戊酸途径在神经元中高度活跃,并且神经元可以在应激性坏死中迅速释放其细胞内物质,导致微环境中许多其他稀有生物分子的水平升高。
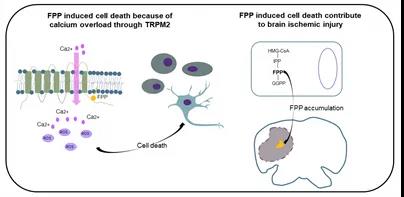
在寻找免疫细胞功能调节剂的过程中,作者意外地发现,当法尼基焦磷酸(FPP)以高浓度存在于细胞外时,会导致细胞迅速而广泛地死亡。FPP带有高电荷的磷酸根和长的疏水烃尾,并且通过依次改变两者发挥对细胞的致死作用,这表明FPP可能与某些互补受体发生特异性相互作用。
研究团队还发现,胞外钙的消耗阻止了FPP的致死作用,通过敲除多种阳离子通道,研究小组发现一种叫做TRPM2的钙离子通道在一定程度上促进了FPP诱导的细胞死亡。通过抑制剂阻断FPP诱导的TRPM2通道的打开,能够抑制FPP诱导的细胞死亡。
论文作者发现,在小鼠缺血性损伤模型中,FPP的浓度会升高,并且预先使用钙通道抑制剂可以减轻损伤程度。此外,通过抑制剂抑制FPP代谢产生,也减轻了损伤程度。
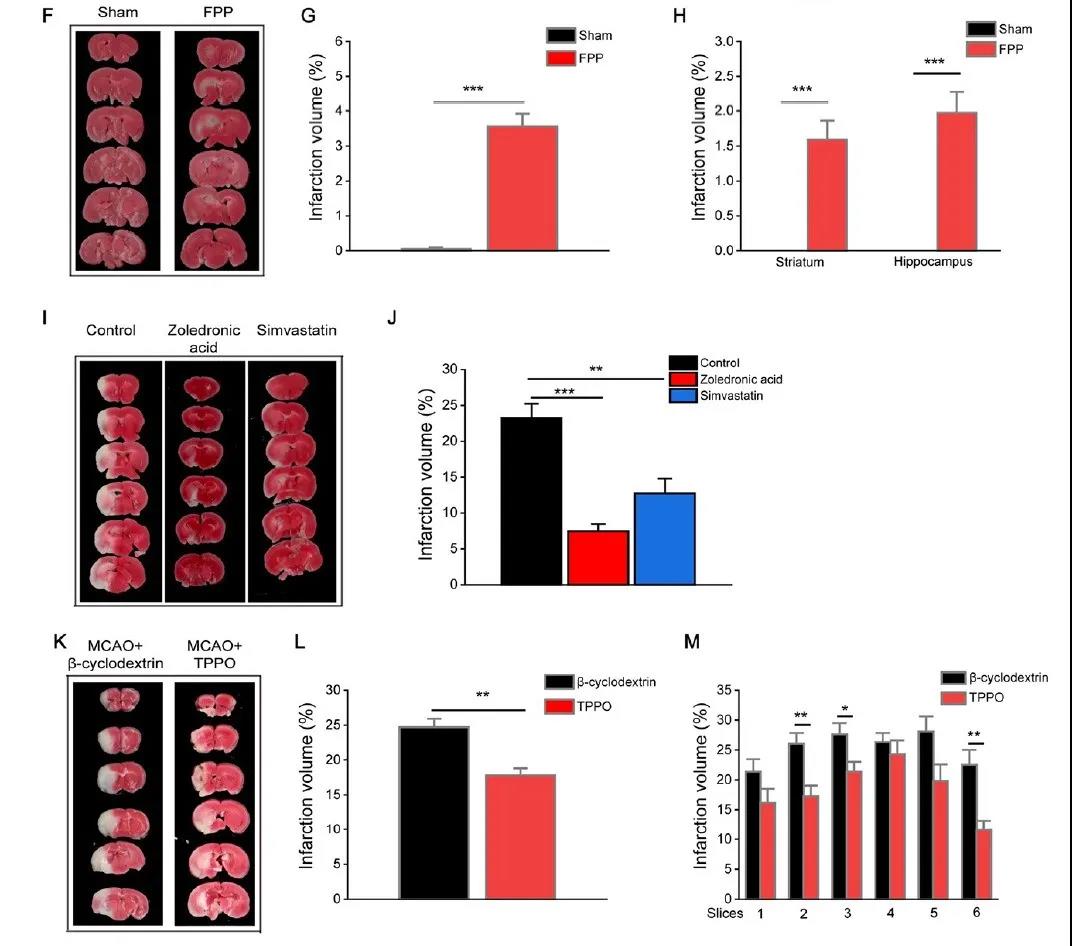
这些结果表明,通过抑制TRPM2,减少钙流入或靶向其代谢合成途径,或阻断FPP的作用,可能是减轻中风损害的新方法。
最后,论文的通讯作者刘万里表示,这些发现为治疗缺血性损伤提供了新的药物治疗靶标,还需要进一步深入了解这种新的细胞死亡途径,以及可进行这类干预方式的窗口时间,鉴于人类缺血性损伤的复杂性,靶向此途径最好与当前疗法结合,以改善治疗效果。
原始出处:
Jing Chen, et al. Farnesyl pyrophosphate is a new danger signal inducing acute cell death. April 26, 2021https://doi.org/10.1371/journal.pbio.3001134
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Bio#
58
#Biol#
46
#PLOS Biology#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
96
#新靶点#
49
#清华#
76
中风是俗称,应该称为缺血性卒中吧
65