神经保护剂的应用,我们是否有章可循?
2018-06-12 医师报 医师报
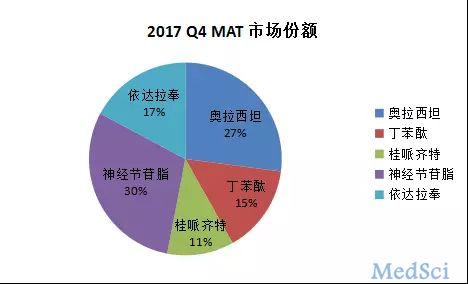
据WHO报告,过去十年全世界导致死亡或引发长期且严重的神经系统疾病的原因里面,卒中排第二位。最新发布的《中国急性缺血性脑卒中诊治指南(2014)》指出,急性缺血性脑卒中特异性治疗的主要手段为:第一,改善脑血循环,进行血管再通,迅速复流以挽救缺血半暗带;第二,神经保护,减少再灌注损伤、抑制缺血级联反应以减轻神经功能缺损。神经保护剂可减小脑梗死面积,无溶栓、抗凝治疗的出血风险,没有严格的时间限制等
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#神经保护#
127
神经保护剂的临床应用效果有待进一步临床论证.
88
学习了
105
学习了受益匪浅
103
好文章.学习获益匪浅.
97
一起学习学习
79
学习了
69