Immunity:免疫树突状细胞囊泡转运的“地图”,揭示抗菌的机制
2016-04-02 中国科学报 中国科学报
近日,第三军医大学科研部生物医学分析测试中心教授万瑛和美国杜克大学免疫学者合作的一项研究,揭开了树突状细胞如何通过蛋白质相互作用完成细胞内囊泡转运以及抗原细胞如何“激活”免疫应答的奥秘。 国际权威期刊《免疫学》(Immunity)杂志刊登了这项研究成果。该研究获得了国家自然科学基金海外及港澳学者研究基金(31028007)、面上项目(31470857)等资助。万瑛表示,正是科学基金对海外及港澳学
近日,第三军医大学科研部生物医学分析测试中心教授万瑛和美国杜克大学免疫学者合作的一项研究,揭开了树突状细胞如何通过蛋白质相互作用完成细胞内囊泡转运以及抗原细胞如何“激活”免疫应答的奥秘。
国际权威期刊《免疫学》(Immunity)杂志刊登了这项研究成果。该研究获得了国家自然科学基金海外及港澳学者研究基金(31028007)、面上项目(31470857)等资助。万瑛表示,正是科学基金对海外及港澳学者研究的资助,让他和杜克大学的研究者有机会合作开展这项研究,从而促进了我国免疫学方面有关囊泡转运的基础科学研究。
瞄准树突状细胞
细胞吞噬作用是机体防御微生物感染的重要机制。上世纪70年代,诺贝尔生理学或医学奖得主拉尔夫·斯坦曼发现,作为一种新型的吞噬细胞,树突状细胞在机体免疫应答过程中发挥着信息交换的作用。
不过,蛋白质等生物大分子不能直接穿过细胞膜,必须依靠膜结构来“穿越”细胞膜。经过长时间的研究,科学家提出了“囊泡转运”的概念,即大分子物质进出细胞的过程由膜包裹、形成囊泡、与膜融合或断裂组成。
树突状细胞则通过复杂的囊泡转运,解析入侵病原体信息,启动获得性免疫。在研究者们看来,能深入了解树突状细胞囊泡转运过程,感染性疾病的治疗就有了科学基础。
万瑛介绍,据世界卫生组织统计,目前每年约有800万由结核分枝杆菌感染引起的结核病例发生,导致上百万人死亡。而结核分枝杆菌、伤寒沙门氏菌和李斯特菌等也严重威胁着人类健康。
“树突状细胞不仅能产生大量与免疫应答有关的细胞因子,还能摄取和处理抗原,进而启动机体免疫应答。”万瑛说,“厘清树突状细胞与病原菌相互作用的细胞生物学基础仍有许多问题需要阐明。”
描绘囊泡转运过程
“想要了解树突状细胞的囊泡转运如何精确完成,就必须知道有哪些蛋白参与到这个过程中以及这些蛋白进行了怎样的相互作用。”
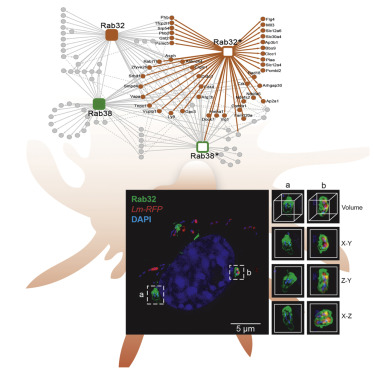
2009年前后,万瑛带领研究小组,采用RNA干扰技术大规模地筛选出与细胞内囊泡转运相关的蛋白家族,发现了12个与树突状细胞“激活”免疫应答有关的蛋白,被称为“Rab”蛋白。相关工作发表在《美国科学院院刊》(PNAS)上。
在此基础上,研究人员又发展了新型串联亲和纯化技术,鉴定了与囊泡转运相关的一种“Rab蛋白”家族的相互作用。
万瑛指出:“我们通过这一结果绘制出一幅描述树突状细胞囊泡转运的‘地图’。”
研究小组详细解析了Rab32蛋白关联网络的功能,发现Rab32-PHB-PHB2蛋白复合体参与树突状细胞清除感染的“李斯特细菌”。这一复合体位于包裹李斯特细菌的囊泡上,能够限制李斯特细菌的复制。
而结合超分辨显微镜和双束扫描电镜技术,研究小组首次发现逃逸吞噬体的李斯特细菌被Rab32阳性囊泡再次包裹,揭示了细胞针对逃逸吞噬体细菌的第二波膜性防御机制。
原始出处:
Li Y, Wang Y, Zou L, Tang X, Yang Y, Ma L, Jia Q, Ni Q, Liu S, Tang L, Lin R, Wong E, Sun W, Wang L, Wei Q, Ran H, Zhang L, Lian H, Huang W, Wu Y, Li QJ, Wan Y. Analysis of the Rab GTPase Interactome in Dendritic Cells Reveals Anti-microbial Functions of theRab32 Complex in Bacterial Containment. Immunity. 2016 Feb 16;44(2):422-37. doi: 10.1016/j.immuni.2016.01.027.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Immunity#
72
#转运#
74
厉害
153
厉害啊
162
#抗菌#
70
#囊泡#
0
有进步,继续努力
132
学习了不错
150