J Allergy Clin Immun:鼻炎有救了!研究发现慢性鼻窦炎的治疗靶点
2020-02-14 小通 生物通
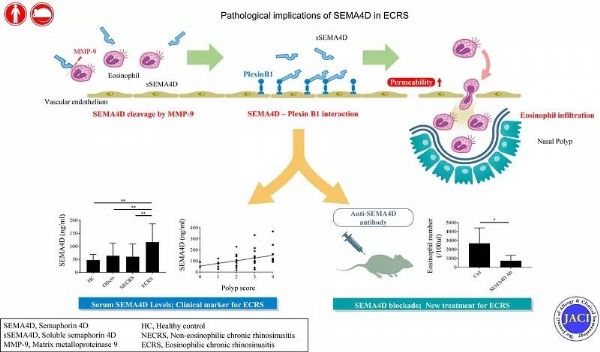
大阪大学的研究人员近日研究了semaphorin蛋白的活性,这是一种细胞表面分子,参与了神经系统的信号传统和免疫分析。他们发现,semaphorin蛋白促进了ECRS患者的过敏反应和鼻息肉的发展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#治疗靶点#
88
期待进展
114
#研究发现#
74
#ALL#
69
#慢性鼻窦炎#
94