Cell Stem Cell:华人科学家找到改变干细胞多能状态的“命运转换器”
2016-06-28 佚名 生物谷
近日,来自美国西奈山医学院的华人科学家Jianlong Wang在国际学术期刊Cell Stem Cell上发表了一项最新研究进展,他们通过研究发现了调节干细胞多能性状态转换的关键分子,对于未来应用干细胞开展再生医学治疗提供了新基础。随着研究不断深入,人们对于细胞多能性的认识也不断增加,根据细胞生长条件可以将多能性定义为不同的细胞状态。虽然已经有研究从分子水平上对原始态多能性和始发态多能性状态进行
近日,来自美国西奈山医学院的华人科学家Jianlong Wang在国际学术期刊Cell Stem Cell上发表了一项最新研究进展,他们通过研究发现了调节干细胞多能性状态转换的关键分子,对于未来应用干细胞开展再生医学治疗提供了新基础。
随着研究不断深入,人们对于细胞多能性的认识也不断增加,根据细胞生长条件可以将多能性定义为不同的细胞状态。虽然已经有研究从分子水平上对原始态多能性和始发态多能性状态进行了描述,但是人们对于不同多能性状态的调控过程中发生的事件仍了解得不够充分。
受精之后大约3到5天,尚未植入子宫(pre-implantation)的胚胎中生成了几十个原始态(naive)胚胎干细胞,这些细胞未来将分化成动物体内所有细胞。当胚胎植入子宫后(post-implantation),原始态干细胞很快迈出向特定细胞类型分化的第一步,变为始发态 (primed)胚胎干细胞。虽然原始态和始发态胚胎干细胞都具有分化成所有其他成体细胞的能力,但是始发态胚胎干细胞更难培养和进行基因操作,分化能力略低且不稳定,因此原始态干细胞对于再生医学的应用价值更高。研究小鼠原始态到始发态胚胎干细胞的转化过程, 不仅可以揭示哺乳动物胚胎发育最早期细胞命运决定的秘密,而且对于再生医学有应用价值,可以帮助人们获得真正的人类原始态胚胎干细胞。
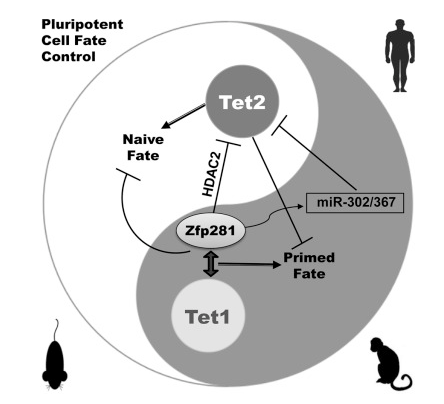
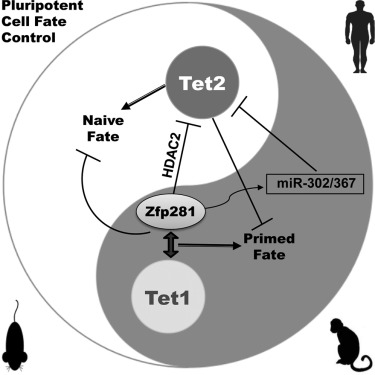
在这项研究中,研究人员对小鼠胚胎干细胞进行了comparative RNA-seq分析,对与原始态多能性和始发态多能性状态相关的多能干细胞命运(PCF)基因特征进行了定义。研究人员发现Zfp281作为始发态多能性状态下一个关键的转录调控因子会阻碍细胞获得原始态多能性,这种情况在小鼠和人类胚胎干细胞中都存在。
研究人员从分子机制上进行了深入研究,他们发现Zfp281能够与Tet1以及它的直接转录靶标miR-302/367发生相互作用,负向调控Tet2表达帮助建立和维持始发态多能性。与之相反,Tet2的异常表达能够有效驱动始发态细胞形成原始态多能性。
这项研究表明Tet1和Tet2在调节干细胞获得不同多能性状态方面具有相反功能,而Zfp281能够通过调节Tet2表达影响干细胞的多能性状态,该研究为获得原始态多能干细胞以及应用干细胞进行再生医学治疗提供了重要信息。
原始出处
Miguel Fidalgo, Xin Huang, Diana Guallar,Carlos Sanchez-Priego, Victor Julian Valdes,Arven Saunders, Junjun Ding, Wen-Shu Wu,Carlos Clavel,Jianlong Wang.Zfp281 Coordinates Opposing Functions of Tet1 and Tet2 in Pluripotent States.Cell Stem Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
57
#CEL#
0
#stem cell#
60
#STEM#
47
#华人#
53