Nat Immunol:itch抑制IL-17介导的肠炎机制
2016-07-18 佚名 生物谷
炎症反应是宿主抵抗微生物侵染以及组织损伤的保护性反应。然而,失去控制的炎症反应容易提高癌症病发与生长的风险。例如,患有IBD以及溃疡性肠炎的患者更加容易患大肠癌。因此,了解大肠炎症反应的机制对于理解大肠癌的发病原因十分重要。越来越多的证据表明IL-17在肠道炎症反应以及肿瘤生成中具有关键的作用,而IL-17在肠道中的特异性表达主要由Th17细胞、γδT细胞以及天然淋巴细胞完成。IL-17能够通过引
炎症反应是宿主抵抗微生物侵染以及组织损伤的保护性反应。然而,失去控制的炎症反应容易提高癌症病发与生长的风险。例如,患有IBD以及溃疡性肠炎的患者更加容易患大肠癌。因此,了解大肠炎症反应的机制对于理解大肠癌的发病原因十分重要。
越来越多的证据表明IL-17在肠道炎症反应以及肿瘤生成中具有关键的作用,而IL-17在肠道中的特异性表达主要由Th17细胞、γδT细胞以及天然淋巴细胞完成。IL-17能够通过引发下游多种细胞因子与趋化因子的表达,招募中性粒细胞与巨噬细胞到炎症部位造成组织损伤。
有研究表明肠道的微生物与局部的细胞因子环境共同促进了IL-23与IL-6的表达,之后进一步提高RORγt的活性,引起IL-17的表达。然而,细胞内部控制RORγt活性并调节IL-17表达的机制目前仍不清楚。
免疫细胞中信号蛋白的翻译后修饰过程主要是泛素化修饰。泛素化的完成需要一系列的酶促反应,包括E1、E2以及E3。Itch是一类泛素连接酶,它的失活伴随着多种器官的炎症紊乱。为了研究itch的缺失对大肠炎症以及大肠癌的发生具有怎样的作用,来自美国贝勒医学院的K Venuprasad课题组进行了深入研究,相关结果发表在最近一期的《natute immunology》杂志上。
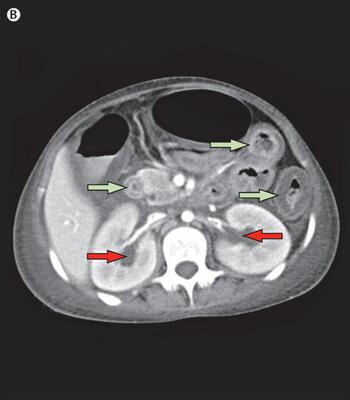
首先作者比较了野生型小鼠与itch突变体小鼠的生理表型。结果显示,突变体小鼠相比野生型其肠炎的发生几率有了明显的提升,同时,突变体小鼠更加容易患大肠癌。进一步,作者发现突变体小鼠肠道的IL-17的表达量有了明显的上升。
为了研究Itch的缺失对IL-17的表达的影响是如何实现的,作者进行了体外实验,结果显示,Itch能够特异性地与细胞因子ROR-γt中的PPXY结构域相互作用。之后,作者发现itch与ROR-γt的结合能够导致后者的泛素化-K48修饰,进而导致ROR-γt的蛋白酶体降解。
之后,作者发现Itch缺失突变体小鼠中ROR-γt的活性确实发生了明显的提高,而且这一缺失突变能够促进小鼠肠道中IL-17的表达。进一步,作者证明itch的缺失引发的ROR-γt泛素化水平的下降能够促进肠道的炎症反应,这些结果共同证明了itch调节ROR-γt活性的作用。
原始出处
Mahesh Kathania, Prashant Khare, Minghui Zeng, Brandi Cantarel, Haiying Zhang, Hideki Ueno & K Venuprasad.tch inhibits IL-17-mediated colon inflammation and tumorigenesis by ROR-γt ubiquitination.Nat Immunol.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
99
#itch抑制#
61
#IL-17#
62
#IL-1#
54