JAMA Netw Open:ER+/HER2-女性乳腺癌患者用或不用他莫昔芬治疗25年生存评估:Stockholm他莫昔芬(STO-3)研究的二次分析
2021-07-01 yd2015 MedSci原创
该研究表明,对于特定患者,肿瘤大小、肿瘤分级跟患者长期生存有关。ER+/HER2-患者中,大肿瘤、低级别、PR阳性患者可以从他莫昔芬中取得长期生存获益。
乳腺癌是女性常见的恶性肿瘤。目前乳腺癌根据分期以及分子分型等进行精准治疗。对于雌激素阳性(ER+)HER2阴性(HER2-)乳腺癌患者中,他莫昔芬是常用的内分泌治疗药物。我们知道临床指标如肿瘤大小,肿瘤分级,激素受体状态以及Ki67等跟患者的短期预后有关。但是这些指标跟患者的长期生存的关系不明确。因此,国外研究团队开展研究评估在绝经后淋巴结阴性的ER+/HER2-乳腺癌患者中服用他莫昔芬这些临床指标跟长期生存的关系。相关研究发表在JAMA Netw Open杂志上。
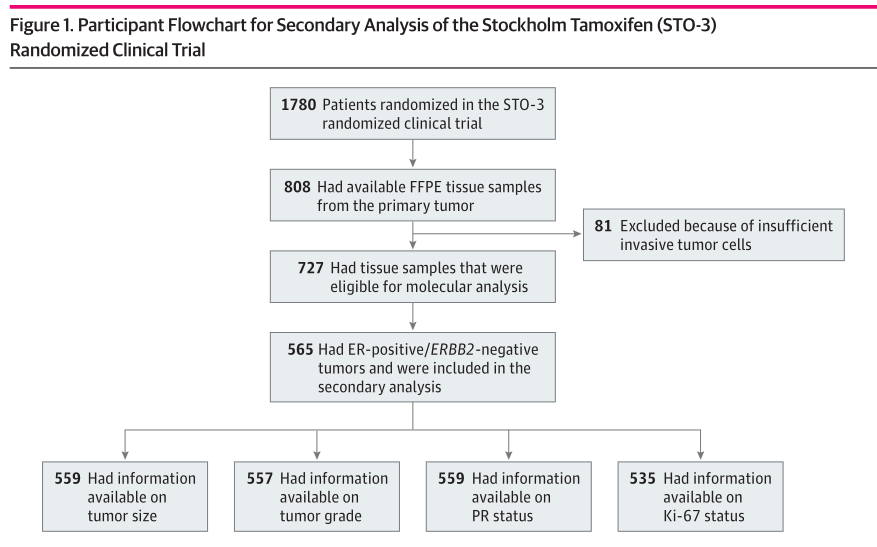
该研究是对Stockholm他莫昔芬(STO-3)随机临床研究中565例女性患者的二次分析。STO-3研究是在1976至1990年开展的,1780例伴有淋巴结阴性的绝经后女性患者随机分配至辅助他莫昔芬治疗或无内分泌治疗。2年治疗无复发者再次随机分配至3年他莫昔芬或无内分泌治疗。
研究概况
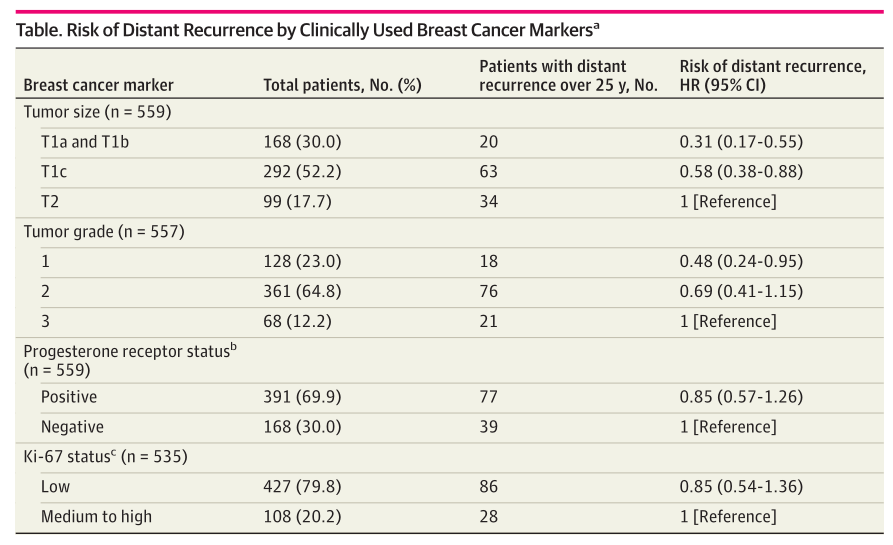
研究包括565例患者,平均年龄为62岁。就肿瘤大小而言,559例患者中,168例(30.0%)为T1a/b,292例(52.2%)为T1c,99例(17.7%)为T2。557例患者中,128例(23.0%)为肿瘤1级,361例(64.8%)为肿瘤2级,68例(12.2%)为肿瘤3级。
T1a/b患者较T1c和T2患者的长期远处无复发间隔(DRFI)更长,分别为88% (95%CI,80%-93%)和76% (95%CI,70%-81%)、63% (95%CI,50%-73%; log-rank P <0 .001)。肿瘤1级、2级和3级患者的长期DRFI分别为81% (95% CI,70%-88%), 77%(95%CI,71%-81%)和77%(95%CI,71%-81%)。但是PR状态和Ki67分层分析对DRFI的影响没有明显差异。
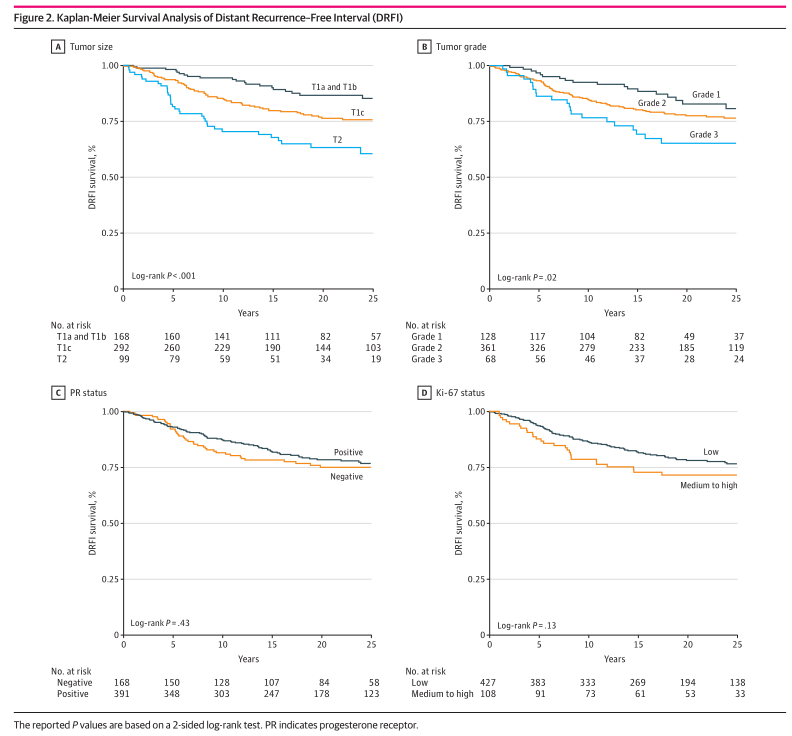
远处无复发间隔(DRFI)分析
多变量Cox回归分析,小肿瘤较大肿瘤远处复发风险更低(T1a/b vs T2,HR=0.31,95% CI, 0.17-0.55; T1c vs T2,HR=0.58, 95%CI, 0.38-0.88)。同样,肿瘤1级患者较3级患者的远处复发风险降低(HR=0.48; 95%CI,0.24-0.95)。但是在2级和3级之间没有明显差异。同样,PR状态和Ki67患者分层分析远处复发风险没有统计学差异。
远处无复发风险
与没有进行内分泌辅助治疗的患者相比,接受他莫昔芬患者中大肿瘤更能获益,T1c患者(HR,0.53[95%CI,0.32-0.89]),T2(HR,0.34[95%CI,0.16-0.73]),但是T1a/b患者没有差异。同样,肿瘤1级患者(HR,0.24[95%CI,0.07-0.82]和肿瘤2级患者(HR,0.50[95%CI,0.31-0.80])能够获益,但肿瘤3级患者没有差异。PR+患者服用他莫昔芬有获益(HR,0.38;95%CI,0.24-0.62)。高Ki-67表达患者(HR, 0.39; 95% CI, 0.17-0.92)和低Ki-67表达患者(HR,0.45;95%CI,0.29-0.71)均可从他莫昔芬中获益。
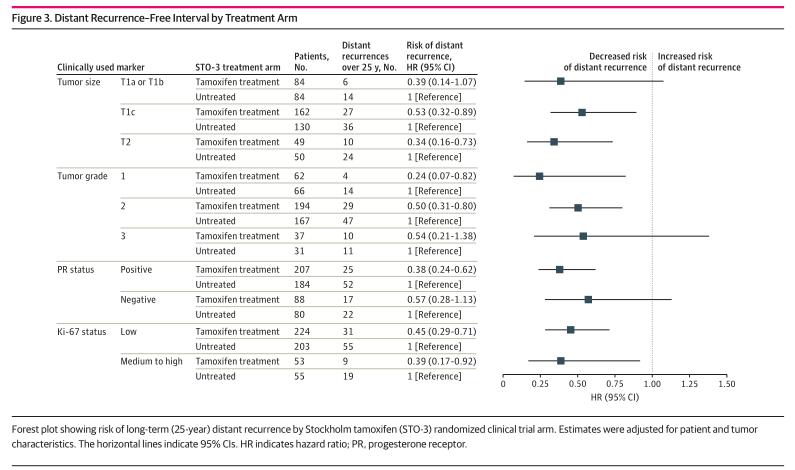
他莫昔芬用药与否获益分层分析
综上,该研究表明,对于特定患者,肿瘤大小、肿瘤分级跟患者长期生存有关。ER+/HER2-患者中,大肿瘤、低级别、PR阳性患者可以从他莫昔芬中取得长期生存获益。
原始出处:
HumaDar; AnnelieJohansson; AnnaNordenskjöld;et al. Assessment of 25-Year Survival of Women With Estrogen Receptor–Positive/ERBB2-Negative Breast Cancer Treated With and Without Tamoxifen Therapy: A Secondary Analysis of Data From the StockholmTamoxifen Randomized Clinical Trial. JAMA Network Open.2021;4(6):e2114904.doi:10.1001/jamanetworkopen.2021.14904.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NET#
48
#HER2-#
64
#PE#
46
学习了
68
#他莫昔芬#
66
#乳腺癌患者#
44
收藏来了
70
收藏了
69
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
86
深度好文
65