共识易览:流感如何合理用药?
2016-04-18 指南君 中华内科杂志
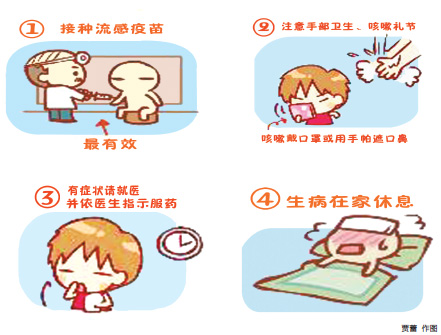
流行性感冒(简称流感)是由流行性感冒病毒引起的急性呼吸道传染病,由于流感病毒(主要是甲型流感病毒)的易变性和不可预知性,常常造成流感的暴发流行,甚至造成全球范围的大流行。 鉴于流感病毒类型的变迁及新药物的上市,中国医师协会呼吸医师分会组织相关专家结合我国流感流行病毒株类型和耐药情况共同编写了"合理应用抗流行性感冒病毒药物治疗流行性感冒专家共识(2016年)",用于指导我国流感患者抗流感病
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了,有用
143
#合理用药#
60
不错的文章
133
值得学习
178
学习了,很好
90
这个知识值得拥有
139