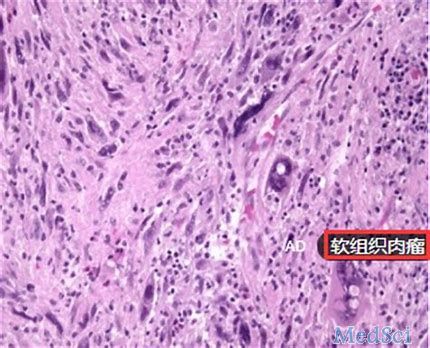
2018年欧洲肿瘤内科学会:NBTXR3在软组织肉瘤中的阳性结果
2018-10-21 MedSci MedSci原创
巴黎居里研究所的肉瘤和复杂肿瘤外科部门负责人Sylvie Bonvalot博士在2018年欧洲肿瘤内科学会上展示了NBTXR3的阳性结果,与单独放疗相比,NBTXR3是第一个显示具有临床益处的放射治疗增强剂。NBTXR3具有新的作用模式,旨在直接破坏肿瘤并激活免疫系统,用于局部控制和全身性疾病治疗。
软组织肉瘤在中老年人发病率较高,无性别差异。可来源于脂肪、筋膜、肌肉、纤维、淋巴及血管,每种都有不同的组织学、生物学特性和不一样的局部浸润和淋巴转移倾向,因此难以治疗。巴黎居里研究所的肉瘤和复杂肿瘤外科部门负责人Sylvie Bonvalot博士在2018年欧洲肿瘤内科学会上展示了NBTXR3的阳性结果,与单独放疗相比,NBTXR3是第一个显示具有临床益处的放射治疗增强剂。NBTXR3具有新的作用模式,旨在直接破坏肿瘤并激活免疫系统,用于局部控制和全身性疾病治疗。
在II期/III期Act.in.sarc研究中,共有180名患有四肢或躯干壁局部晚期软组织肉瘤的成年患者,以1:1的比例随机分配至(i)A组,以推荐剂量接受单次瘤内注射NBTXR3,然后进行放射治疗或(ii)对照组B组,单独用放射疗法进行治疗。在两组中,放疗后进行手术。结果显示,与单独放疗相比,NBTXR3具有显著的临床益处。
原始出处:
http://www.firstwordpharma.com/node/1598712#axzz5UXJIsme7
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#NBTXR3#
61
#肿瘤内科#
67
#欧洲肿瘤内科学会#
61
#阳性结果#
62
#欧洲#
58
#软组织#
64