妇产科学之最 知识点汇总 !
2016-08-15 佚名 医学之声
.子宫肌瘤是女性生殖器最常见的良性肿瘤。84.肌瘤变性,玻璃样变最常见。85.经量增多及经期延长是子宫肌瘤最常见的症状。86.子宫内膜癌,以来源于子宫内膜腺体的腺癌最常见。87.子宫内膜癌,绝经后以及绝经过渡期异常阴道流血为最常见的症状,诊断性刮宫为最常用的诊断方法。早期首选手术治疗。88.子宫肉瘤,最常见的症状为阴道不规则流血伴腹痛,确诊依据是组织学诊断。89.原发性平滑肌肉瘤是子宫最常见的恶性
1.性成熟期是卵巢生殖功能与内分泌功能最旺盛的时期。
2.孕酮在排卵后7~8日黄体成熟时分泌量达最高峰。
3.卵巢周期使女性生殖器发生一系列周期性变化,尤以子宫内膜的周期性变化最为显著。
4.子宫内膜间质水肿在增殖中期最为明显。
5.在月经周期中,阴道粘膜呈现周期性改变,这种改变在阴道上段最明显。
6.排卵前,阴道上皮表层细胞出现角化,其程度在排卵期最明显。
7.将宫颈黏液作涂片检查,干燥后可见羊齿植物叶状结晶,这种结晶在月经周期第6~7日开始出现,到排卵期最为清晰和典型。
8.hCG在受精后10日可自母亲血清中测出,为诊断早孕最敏感的方法。
9.子宫是妊娠期及分娩后变化最大的器官。
10.心排出量增加为孕期循环系统最重要的改变。
11.停经是妊娠最早的症状,但不是妊娠的特有症状。
12.正常情况下,子宫高度在妊娠36周时最高。
13.纵产式占足月妊娠分娩总数的99.75%。
14.胚胎着床后31%发生自然流产,其中80%为早期流产,在早期流产中,约2/3为隐性流产。
15.胚胎或胎儿染色体异常是早期流产最常见的原因。
16.流产时胚胎发育异常,一类是全胚发育异常,另一类是特殊发育缺陷,以神经管畸形、肢体发育缺陷最常见。
17..输卵管妊娠占异位妊娠95%左右,其中壶腹部妊娠最常见,约占78%。
18.早产中自发性早产是最常见的类型。
19.子痫是妊娠期高血压疾病最严重的阶段,是妊娠期高血压疾病所致母儿死亡的最主要原因。
20.硫酸镁是治疗子痫及预防复发的首选药物。
21.脑血管意外是子痫患者死亡的最常见原因。
22.血清胆汁酸升高是妊娠期肝内胆汁淤积症的最主要实验室证据。
23.糖尿病孕妇中90%以上为妊娠期糖尿病。
24.妊娠合并心脏病在我国位居非直接产科死因首位。
25.分娩期为心脏负担最重的时期。(人人网河北医大学习吧)
26.从妊娠、分娩及产褥期对心脏的影响来看,妊娠32~34周后、分娩期(第一产程末、第二产程)、产后3日内心脏负担最重是心脏病孕妇的危险时期,极易发生心脏衰竭。
27.目前在妊娠合并心脏病患者中,先天性心脏病占35~50%,位居第一。
28.房间隔缺损是最常见的先天性心脏病,占20%左右。
29.右向左分流型先天性心脏病临床上以法洛四联症及艾森曼格综合征最常见。
30.风湿性心脏病中二尖瓣狭窄最常见。
31.心力衰竭最容易发生在妊娠32~34周、分娩期及产褥早期。
32.乙型病毒性肝炎最常见。河北医大学习吧
33.缺铁性贫血是妊娠期最常见的贫血,占妊娠期贫血的95%。
34.肾上腺皮质激素是治疗ITP的首选药。
35.ITP孕妇的最大危险是分娩时出血。
36.前置胎盘是妊娠晚期严重并发症之一,也是妊娠晚期阴道流血最常见的原因。
37.胎盘早剥是妊娠晚期发生凝血功能最常见的原因,约1/3伴有死胎患者可发生。
38.缩宫素与前列腺素是促进宫缩最直接因素。
39.宫缩以宫底部最强最持久。
40.中骨盆平面为骨盆最小平面,是骨盆最狭窄部分。
41.双顶径为两侧顶骨隆突间的距离,是胎头最大横径。
42.临床上枕先露占95.55%~97.55%,以枕左前位最多见。
43.检测宫缩最简单的方法是助产人员将手掌放于产妇腹壁上,宫缩时宫体部隆起变硬,间歇期松弛变软。
44.胎儿监护仪有两种类型,其中外监护最常用,适用于第一产程任何阶段。
45.新生儿阿普加评分以呼吸为基础,皮肤颜色最灵敏,心率是最终消失的指标。
46.枕后位经阴道最常见分娩方式:若胎头俯屈较好,胎头继续下降至前囟先露抵达耻骨联合下时,以前囟为支点,胎头继续俯屈使顶部及枕部自会阴前缘娩出。
47.臀先露是最常见的异常胎位,占妊娠足月分娩总数的3%~4%。
48.臀先露分单臀先露(最多见),完全臀先露(较多见),不完全臀先露(较少见)。
49.臀先露若未衔接,胎心在脐左(或右)上方听得最清楚。衔接后,胎心听诊在脐下最明显。
50.肩先露是最不利于分娩的胎位。
51.肩先露胎心在脐周两侧最清楚。(人人网河北医大学习吧)
52.肩先露中忽略(嵌顿)性肩先露为最不利的胎位。
53.复合先露,临床以一手或一前臂沿胎头脱出最常见,多发生于早产者。
54.头位难产最常见,但最难诊断。
55.产后出血居我国产妇死亡原因首位。
56.子宫收缩乏力是产后出血最常见原因。首选治疗为子宫按摩和应用缩宫剂。
57.子宫破裂最常见原因是子宫瘢痕及梗阻性难产。
58.产褥期子宫变化最大。
59.产褥感染,B-溶血性链球菌是最常见的病原体,致病性最强。
60.产褥早期发热的最常见原因是脱水,但在2~3日低热后突然出现高热,应考虑感染可能。
61.对产后发热者应首先考虑产褥感染,再考虑产褥病率的其他疾病。
62.晚期产后出血以产后1~2周发病最常见。
63.晚期产后出血,胎盘、胎膜为阴道分娩最常见的原因。
64.产褥期抑郁症是产褥期精神综合征最常见的一种类型。
65.双合诊是盆腔检查中最重要的项目。
66.围绝经期妇女出现阴道流血,以无排卵性功能失调性子宫出血最多见,但应首先排除生殖道恶性肿瘤。
67.外阴阴道假丝酵母菌和滴虫阴道炎是引起外阴瘙痒最常见的原因。
68.外阴鳞状上皮增生是最常见的外阴上皮非瘤样病变。
69.外阴硬化性苔藓可发生于任何年龄,但以绝经后妇女最多见,其次为幼女。
70.外阴及阴道炎症是妇科最常见疾病,各年龄组均可发病。
71.盆腔炎性疾病,炎症部位可局限于一个部位,也可同时累及几个部位,以输卵管炎、输卵管卵巢炎最常见。
72.急性盆腔结缔组织炎,以宫腔结缔组织炎最常见。
73.生殖器结核,血行转移为最主要的传播途径。
74.输卵管结核占女性生殖器结核的90%~100%。
75.子宫内膜病理检查是诊断子宫内膜结核最可靠的依据。
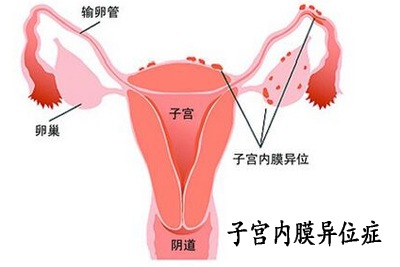
76.子宫内膜异位症绝大多数位于盆腔脏器和壁腹膜,以卵巢、宫骶韧带最常见。
77.腹腔镜检查是目前公认的内异症诊断的最佳方法。
78.子宫颈癌是最常见的妇科肿瘤。
79.子宫颈癌病理类型主要为鳞癌,其中外生型最常见。
80.子宫颈腺癌最常见的是黏液腺癌。
81.子宫颈活组织检查是确诊子宫颈鳞状上皮内瘤变的最可靠方法。
82.子宫颈癌直接蔓延最常见。(人人网河北医大学习吧)
83.子宫肌瘤是女性生殖器最常见的良性肿瘤。
84.肌瘤变性,玻璃样变最常见。
85.经量增多及经期延长是子宫肌瘤最常见的症状。
86.子宫内膜癌,以来源于子宫内膜腺体的腺癌最常见。
87.子宫内膜癌,绝经后以及绝经过渡期异常阴道流血为最常见的症状,诊断性刮宫为最常用的诊断方法。早期首选手术治疗。
88.子宫肉瘤,最常见的症状为阴道不规则流血伴腹痛,确诊依据是组织学诊断。
89.原发性平滑肌肉瘤是子宫最常见的恶性间叶性肿瘤。
90.大约10%的子宫内膜癌与遗传有关,其中最密切的遗传症候群是林奇综合征,也称遗传非息肉结直肠癌综合征。
91.术后放疗是1期G1和2期内膜癌最主要的术后辅助治疗。
92.卵巢组织成分非常复杂,是全身各脏器原发肿瘤类型最多的器官。
93.直接蔓延:外观肿瘤局限在原发部位,也可存在广泛微转移,其中以上皮性癌最为典型。
94.淋巴转移:横膈为转移的好发部位,尤其右膈下淋巴丛密集,最易受侵犯。
95.滤泡囊肿和黄体囊肿是育龄期妇女最常见的卵巢瘤样病变。
96.卵巢癌最重要的预后因素是肿瘤期别和初次手术后残存灶的大小。
97.卵巢上皮性肿瘤是最常见的卵巢肿瘤。
98.完全性葡萄胎,停经后阴道流血为最常见的症状。
99.转移性滋养细胞肿瘤,最常见的转移部位是肺。
100.超声检查,是诊断子宫原发病最常用的方法。
101.单纯性增生为最常见的子宫内膜增生类型。
102.无排卵性宫血患者临床上最常见的症状是子宫不规则出血,表现为月经周期紊乱,经期长短不一,经期不定或增多,甚至大出血。
103.继发性闭经发生率明显高于原发性闭经,以下丘脑性闭经最常见。
104.Asherman综合征为子宫性闭经最常见原因。
105.垂体性闭经,垂体肿瘤最常见的是分泌PRL的腺瘤。
106.低促性腺激素性腺功能减退,最常见为体质性青春发育延迟。
107.氯米芬是最常用的促排卵药物。
108.含铜宫内节育器是目前我国应用最广泛的IUD。
109.经腹输卵管结扎术是国内应用最广的绝育方法。
110.阴茎套是哺乳期选用的最佳避孕方式。
111.成熟指数(MI)是阴道细胞学卵巢功能检查最常用的一种。
112性活跃妇女的HPV感染率最高,感染的高峰年龄在18~28岁。
113.CA125是目前世界上应用最广泛的卵巢上皮性肿瘤标志物。
114.p53是研究最广泛的人类肿瘤抑制基因。
115.诊断性刮宫是诊断宫腔疾病最常用的方法。
116.雄激素是调节女性性功能最重要的性激素。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#妇产科学#
59
妇产科知识之最和缘由总结很全
89
#知识点#
60
关注值得,学习。赞!好文探究。
89
深度好文,赞一个!!!
76
汇总的全面
83
太好了
87
喜欢这种总结
0
学习了,赞一个!
47
学习了,赞一个!
0