Eur Heart J:股动脉路径与桡动脉路径行PCI对预后的影响——CHAMPION PHOENIX临床实验
2015-09-29 张旭栋译 MedSci原创
美国波士顿布列根和妇女医院Gutierrez JA等人研究了股动脉路径或桡动脉路径行PCI与坎格雷洛合用对于预后结局的影响,其成果发表中9月份 European heart journal期刊上。目的:CHAMPION PHOENIX临床实验中,评估股动脉路径和挠动脉路径经皮冠状动脉介入术(PCI)与坎格雷洛(P2Y12抑制剂,)合用的安全性和有效性。方法和结果:研究纳入11 145例患者,双盲双
美国波士顿布列根和妇女医院Gutierrez JA等人研究了股动脉路径或桡动脉路径行PCI联合坎格雷洛对预后结局的影响,其成果发表中9月份 European heart journal期刊上。
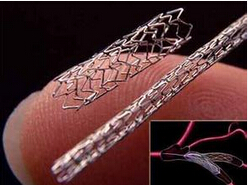
目的:CHAMPION PHOENIX临床实验中,评估股动脉路径和挠动脉路径经皮冠状动脉介入术(PCI)与坎格雷洛(P2Y12抑制剂,)合用的安全性和有效性。
方法和结果:研究纳入11 145例患者,双盲双模拟随机分配一片坎格雷洛和行PCI术的2小时输注坎格雷洛或氯吡格雷。主要终点:48小时内死亡,心肌梗死,缺血血管重建或支架内血栓形成,和主要安全终点为开通闭塞冠状动脉策略的全球性研究(GUSTO)定义的严重出血。行PCI术和接受药物治疗的患者中,接受了股动脉PCI术的患者有8064(74%)例,接受了桡动脉PCI术的患者有2855(26%)例。在股动脉路径组队列中,坎格雷洛和氯吡格雷主要终点率分别为4.8%与6.0%(比值比OR [95%可信区间] = 0.79 [0.65-0.96]);桡动脉路径队列中,坎格雷洛和氯吡格雷主要终点率分别为4.4%与5.7%(OR [95%CI = 0.76 [0.54-1.06]),P-相互作用为0.83。股动脉路径队列中,使用坎格雷洛和氯吡格雷所致的GUSTO严重出血率分别为0.2%和0.1%(OR [95%CI] = 1.73 [0.51-5.93])。桡动脉路径队列中,使用坎格雷洛和氯吡格雷所致的GUSTO严重出血率分别为0.1%和0.1%(或[95%CI] = 1.02 [0.14-7.28]),P-相互作用为0.65。股动脉路径中,使用更敏感的ACUITY定义的出血评估,使用坎格雷洛和氯吡格雷所致的出血率分别为5.2%和3.1%(OR [95%CI = 1.69 [1.35-2.12]);挠动脉路径中,使用更敏感的ACUITY定义的出血评估,使用坎格雷洛和氯吡格雷所致的出血率分别为1.5%和0.7%(OR [95%CI] = 2.17 [1.02-4.62],P-相互作用0.54)。
结局:CHAMPION PHOENIX试验中,坎格雷洛能减少缺血事件,不会显著增加GUSTO定义的严重出血结局。不论出血率的定义如何,都显示桡动脉路径行PCI出血率更低。
原文出处:
Gutierrez JA, Harrington RA, Blankenship JC,et al.The effect of cangrelor and access site on ischaemic and bleeding events: insights from CHAMPION PHOENIX. European heart journal. 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#股动脉路径#
49
#CHAMPION#
60
#股动脉#
53
#临床实验#
0
经桡动脉途径pci并发症大大减少
144
#ART#
62
#桡动脉#
58
#HEART#
56