Eur Urol:考虑进行前列腺手术男性的下尿路症状诊断评估
2020-07-19 AlexYang MedSci原创
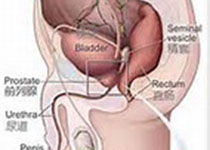
前列腺手术能通过减轻膀胱出口梗阻(BOO)来改善下尿路症状(LUTS)。然而,在没有BOO或者逼尿肌活动低下的情况下手术的效果一般。尿动力学(UDS)能够对BOO进行鉴定,且还能测量逼尿肌活性,但是在
前列腺手术能通过减轻膀胱出口梗阻(BOO)来改善下尿路症状(LUTS)。然而,在没有BOO或者逼尿肌活动低下的情况下手术的效果一般。尿动力学(UDS)能够对BOO进行鉴定,且还能测量逼尿肌活性,但是在临床实践中缺乏相关证据。
最近,有研究人员评估了是否包含UDS的护理能够在不增加泌尿症状的情况下减少手术。研究进行的时间为2014年10月和2016年12月之间,820名男性(平均年龄为68岁)随机分为常规护理(RC)组(n=393)和UDS组(n=427)。研究发现,UDS组的IPSSs均值表现出了非劣性(UDS 12.6; RC 13.1; 第18个月调整后差异:-0.33 (95%CI -1.47, +0.80))。在UDS组,153/408(38%)接受了手术,RC组中为138/384(36%)(调整后OR:1.05; 95% CI 0.77, 1.43)。副作用事件共记录428起(UDS 234; RC 194),包括了两组之间相似的事件和11例不相关的死亡。
最后,研究人员指出,UDS组在IPSS方面与RC组相比表现出了非劣性,但是并未减少手术比例。研究表明了UDS在非复杂性LUTS评估中的常规使用作用有限,可选择性使用。
原始出处:
Marcus J Drake , Amanda L Lewis , Grace J Young et al. Diagnostic Assessment of Lower Urinary Tract Symptoms in Men Considering Prostate Surgery: A Noninferiority Randomised Controlled Trial of Urodynamics in 26 Hospitals. Eur Urol. 29 June 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#下尿路#
60
#尿路症状#
68
#下尿路症状#
72
学习
117