糖尿病患者肿瘤患病率明显增高(REACTION研究)
2017-03-19 谭嘉 健康报
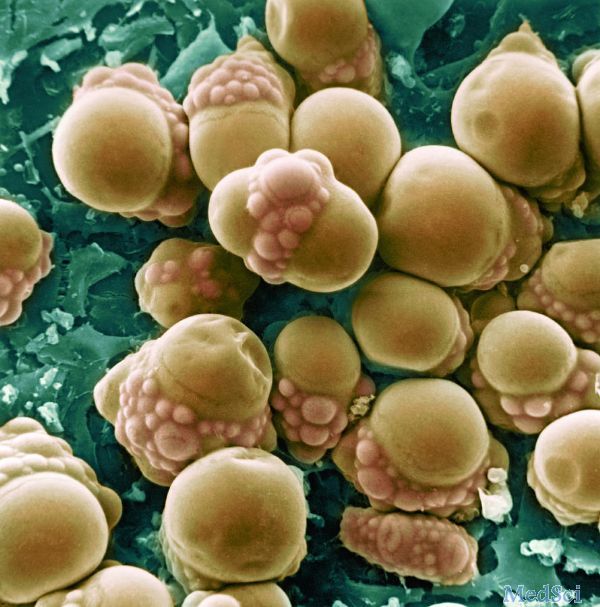
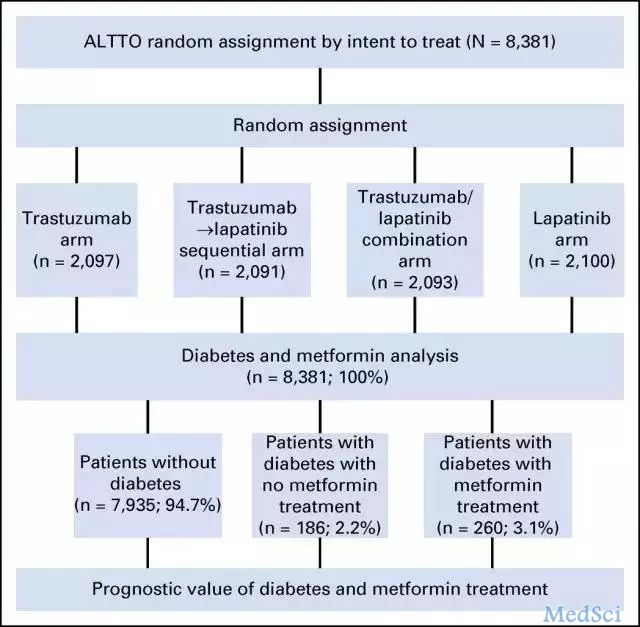
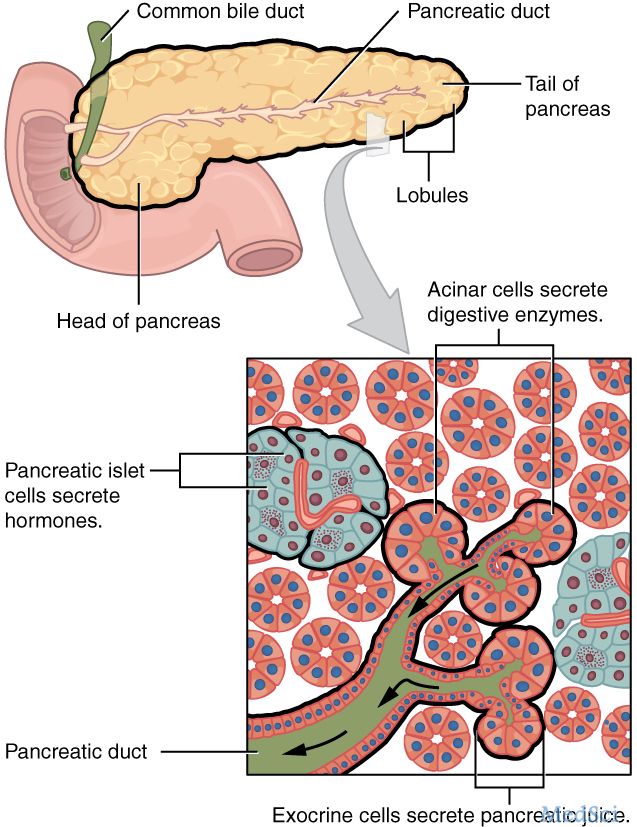
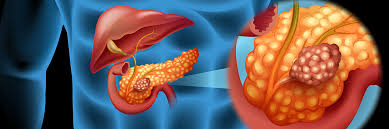
我国一项涉及25万余人的多中心、前瞻性观察研究结果显示,糖代谢异常与部分恶性肿瘤风险增加显着相关,糖尿病病程、胰岛素抵抗也与部分恶性肿瘤患病风险增加相关。在近日于江苏省无锡市举行的2017华东内分泌代谢病论坛上,专家提醒,临床医生和糖尿病患者在控制血糖的同时,也要重视相关肿瘤好发部位的年度体检。据介绍,上海交通大学医学院附属瑞金医院宁光教授,牵头开展了中国2型糖尿病患者肿瘤发生风险的流行病学注册研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ReACT#
60
#患病率#
64
#糖尿病患者#
53
#增高#
65
#增高#
64
学习了,很有用的!!!
104
学习了谢谢了。
82
学习了很有用
86
跟肝癌关系大不?
96
糖代谢异常与部分恶性肿瘤风险增加显着相关
96