JAMA子刊:转移性透明细胞肾细胞癌患者行细胞减灭性肾切除术后的生存结局如何?
2022-05-31 liangying MedSci原创
工具变量分析没有证明细胞减灭性肾切除术对转移性ccRCC患者具有生存优势。
一级证据未能证明现代转移性肾透明细胞癌(ccRCC)患者行细胞减灭性肾切除术的总体生存率(OS)优势,与很多观察研究报告的这些手术相关的显著OS益处不一致。这些观察性研究并不是为了调整未测量的混杂因素。本研究的目的是评估细胞减灭性肾切除术是否与转移性ccRCC患者的OS改善相关。
这项队列研究在2006年1月1日至2016年12月31日的国家癌症数据库中确定了接受全身靶向治疗的转移性ccRCC患者。分析于2021年7月23日完成。
主要结果是从诊断日期到死亡或最后随访时审查的OS。对选择偏差、多变量Cox比例风险回归和倾向评分匹配进行常规调整以进行比较。所有分析中校正的测量协变量包括年龄、性别、种族、Charlson-Deyo评分、设施类型、诊断年份、临床T分期和临床N分期。
最终研究人群包括12766名患者(中位年龄63岁;IQR 56-70岁,8744(68%)名男性,11206(88%)名白人)。其中,5005例(39%)患者行细胞减灭性肾切除术。对选择偏倚的常规调整表明,细胞减灭性肾切除术显著提高了OS(多变量Cox比例风险回归:风险比[HR],0.49;95%CI,0.47-0.51;倾向评分匹配:HR,0.48;95%CI,0.46-0.50)。工具变量估计值未证实细胞减灭性肾切除术与OS之间的相关性(HR,0.92;95%CI,0.78-1.09)。
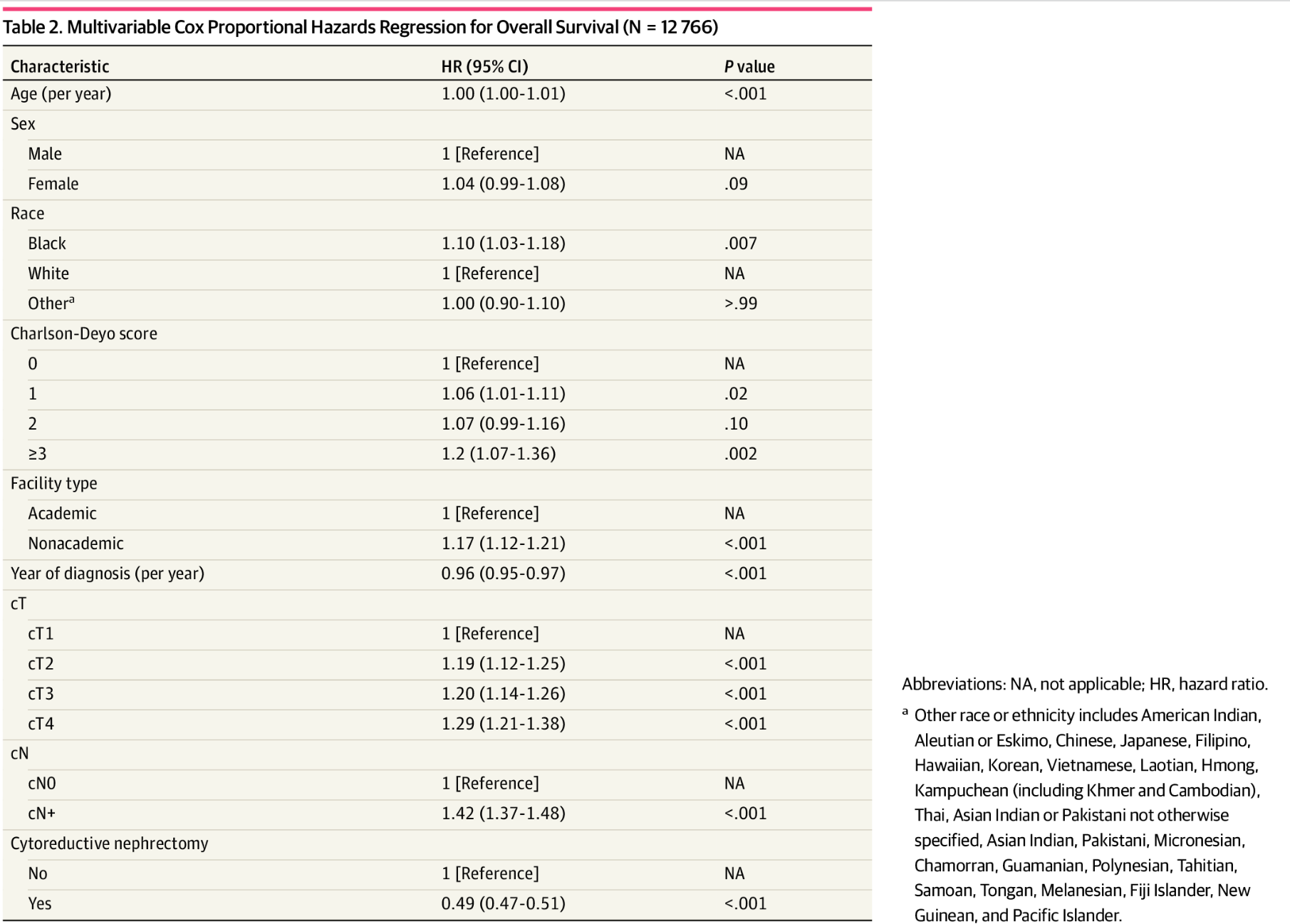
总生存期的多变量Cox比例风险回归(N = 12766)
工具变量分析没有证明细胞减灭性肾切除术对转移性ccRCC患者具有生存优势。这种差异可能反映了这样一个事实,即细胞减灭性肾切除术的手术指征主要是由一些观察数据集中在不常用测量因素所驱动的。
参考文献:Chakiryan NH, Gore LR, Reich RR, et al. Survival Outcomes Associated With Cytoreductive Nephrectomy in Patients With Metastatic Clear Cell Renal Cell Carcinoma. JAMA Netw Open. 2022;5(5):e2212347. doi:10.1001/jamanetworkopen.2022.12347
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肾切除术#
72
#切除术#
55
#细胞癌#
64
签到
54
好文章,谢谢分享。
80
#转移性#
75
JAMA上文章都是顶级的,谢谢梅斯及时上新
63