2017年12月12日,李克强总理探访武汉协和医院,仔细询问肿瘤专家攻克癌症的最新研究和临床进展情况,明确表示要汇聚优势科研力量集中攻关癌症难关,让更多患者和家属早日走出疾病阴影。特此梳理2017年年度国际上抗癌新进展,以飨读者。
世卫组织最新公布数据表明,全球每年880万人死于癌症,占全球每年死亡总人数近六分之一。每年1400多万新发癌症病例,预计到2030年将增加到2100多万。癌症治疗始终是医学上的一个难题,长期以来,科学家们在研究癌症诊断途径、开发治疗和预防癌症新型方法上花费了大量的精力,随着科学家们研究的深入及多种机制的发现,癌症逐渐变成了一种可控的疾病。
癌症诊断进展
癌症诊断领域是全球科学家们研究关注的重点,近年来随着研究的深入,许多新型的癌症检测技术不断涌现。
人工智能正在改变癌症诊断
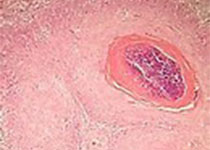
今年年初,谷歌研发出用于乳腺癌诊断的人工智能(AI)系统。这套系统分析了大量的病理组织显微图像,速度比人类快得多,且肿瘤检出率高达92.4%。
如果能够通过检测较早发现结直肠癌,这一癌症甚至被认为“是高度可治愈的”。近日,日本昭和大学的一项研究表明,AI辅助系统有望在良性肿瘤变成恶性之前就检测出结直肠癌,准确率高达86%。这是人类第一次使用和研究AI来完成癌症检测。
尿液检测发现早期癌症
日本名古屋大学等机构的研究人员利用纳米线材料,发明出一种新的检测技术,能够从1ml尿液中检测出约1000种微核糖核酸。利用这种技术分析癌症患者的尿液,发现某些特殊的微核糖核酸出现了异常现象,且与肺癌、肝癌、膀胱癌、前列腺癌等几种癌症的患病特征相关。研究者认为,今后可以利用这一方法,通过检测尿液,形成早期发现癌症生物标记。
新型液体活检创癌症诊疗新纪元
美国西达赛奈医疗中心和加州大学洛杉矶分校的研究团队正在使用一种新型血液分析设备——NanoVelcro芯片,根据循环血液中的肿瘤细胞诊断并追踪前列腺癌等癌症进程。利用液体活检(又称“血液活检”)技术进行癌症诊断,能够减少对穿刺或手术活检等侵入性检查的需要。研究者认为肿瘤检测应该与血液测试一样简单,就像检查血压和体重一样,那才是医学的未来。
癌症治疗进展
数十年来,癌症的治疗手段主要有三种:手术治疗、化疗和放疗,这套铁三角疗法形象地称为“尖刀、毒药和烙铁”。研究新的治疗手段,是攻克癌症难关的必经之路。
免疫新药物相继面世 有望治愈癌症
免疫疗法是通过改造人体的免疫系统,使免疫系统特异性攻击肿瘤来发挥抗癌作用。以PD-1/PD-L1抗体、CAR-T为代表的免疫疗法为人类对抗癌症提供了新的“武器”。
CAR-T细胞疗法是通过特异性识别癌细胞上的抗原来发挥作用,今年8月30日,人类历史上批准的首款CAR-T疗法正式上市,用于治疗复发或难治性(r/r)儿童和年轻成人B细胞急性淋巴细胞白血病。随后多个CAR-T疗法的相继获批上市,为许多血液癌症及个别实体瘤患者,带来了治疗甚至治愈的希望。
表观遗传新疗法 治疗癌症更精准
表观遗传学在癌症特征中发挥的影响已经获得了科学家、医生和制药业的广泛关注。
近日,美国Genentech公司的研究人员鉴别出一种关键酶类,该酶能够通过对细胞染色质进行表观遗传学修饰,促进胰腺癌细胞恶性转化,靶向作用该酶类或能有效促进胰腺癌细胞对当前疗法变得敏感。美国约翰霍普金斯Kimmel癌症中心的研究人员发现,将几种表观遗传治疗药物联合使用,对非小细胞肺癌进行治疗,能够让其更好地响应免疫疗法。
越来越多的证据显示癌症表观遗传学和癌症免疫学相互依赖。因此,免疫治疗和表观遗传治疗的组合疗法将是抗癌药物发展的下一个前沿。
癌症疫苗进展
随着癌症研究的深入,科学家们发现可以通过研发癌症疫苗来实现癌症的预防和治疗,这也成为人类攻克癌症的新阵地。
今年宫颈癌疫苗希瑞适获得了中国食品药品监督管理总局的上市许可。其实除了宫颈癌,许多癌症也有望通过疫苗来进行防治。
RNA疫苗助力免疫系统预防癌症
德国美茵茨大学的研究利用免疫系统对病毒感染的反应,开发出一种纳米粒子RNA疫苗。疫苗通过静脉注射进入体内,在实验鼠和3位晚期黑色素瘤患者身上成功诱发了抗癌免疫反应。该研究为通用癌症疫苗的出现铺平了道路,有望让癌症免疫疗法成为现实。
美国加利福尼亚大学圣地亚哥分校医学院的研究者发现,在癌前阶段将特定的双链RNA注入肝癌模型小鼠的体内,可启动先天免疫系统,阻止小鼠肝癌细胞的生长。研究认为可能存在一种疫苗,可对肝癌高危人群癌症的发生产生一定的预防作用。
新疫苗有效抗击HER2阳性乳腺癌
有数据显示,HER2阳性乳腺癌在所有人类乳腺癌中占20%~30%,是最为凶险的乳腺癌。丹麦哥本哈根大学和意大利博洛尼亚大学的研究人员开发一种新的疫苗技术可以对抗小鼠HER2阳性乳腺癌。此外,华中科技大学等研究单位的科学家们发现,将HER2阳性乳腺癌抗原装载入硅微粒,可大幅度提高疫苗的效力。开发一种抵御HER2的癌症疫苗,或可帮助机体免疫系统识别并摧毁过表达HER2的癌细胞,同时也不会对健康细胞带来任何副作用。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#癌症死亡#
49
学习了受益匪浅
89
非常好的文章.学习了
104
henhao
95
谢谢分享.学习了
89
学习了新知识
104