PLoS One:在法布里病病人中,心脏和肾脏功能障碍与晚期听力损失相关
2017-11-25 AlexYang MedSci原创
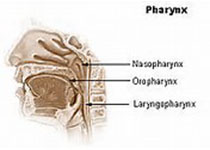
法布里疾病(FD)是一种X染色体连锁的隐性遗传性溶酶体储存障碍,并且能够导致糖鞘脂(Gb3)在肾脏和心脏组织中的积累以及在中央和周围神经系统中的积累。除了明显的肾脏和心脏器官的参与之外,耳蜗症状比如高频听力损失和耳鸣经常能够出现,并且到目前为止没有全面的可利用资料来阐释这种现象。最近,有研究人员在患有FD的病人中,依据心脏和肾脏功能调查了听力损失的情况。研究人员在2012年和2016年之间招募了6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Plos one#
79
#听力#
76
#功能障碍#
63
不错的文章值得推荐
84
不错的文章值得推荐
86
不错的文章值得推荐
102