Advanced Materials:新技术可以捕捉和保存血液循环中的癌细胞
2013-01-04 Advanced Materials 互联网 ssnhwang
2012年12月17日,来自日本理化研究所高等理工学院和洛杉矶加州理工大学的科学家报道了一项研究结果:一种全新的类似于尼龙搭扣样的纳米级装置可以捕捉和释放从原发肿瘤上脱落并进入血液循环的肿瘤细胞。这种新纳米技术可以用来进行肿瘤诊断和为研究癌症如何蔓延到整个身体的机制提供更深刻的理解。该设备提供了一个简便和非侵入性的诊断转移癌的检查方法,可以替代当前的活检。 肿瘤细胞在远离原发肿瘤部位种植形成肿瘤
2012年12月17日,来自日本理化研究所高等理工学院和洛杉矶加州理工大学的科学家报道了一项研究结果:一种全新的类似于尼龙搭扣样的纳米级装置可以捕捉和释放从原发肿瘤上脱落并进入血液循环的肿瘤细胞。这种新纳米技术可以用来进行肿瘤诊断和为研究癌症如何蔓延到整个身体的机制提供更深刻的理解。该设备提供了一个简便和非侵入性的诊断转移癌的检查方法,可以替代当前的活检。
肿瘤细胞在远离原发肿瘤部位种植形成肿瘤前,医生可以通过该设备检测到循环中的肿瘤细胞。该设备还使研究人员保存肿瘤细胞并随后进行研究。
该设备由日本理化学研究所高等理工学院Hsiao-hua Yu和洛杉矶加州理工大学分子和临床药理学系Hsian-Rong Tseng领导的团队研发。该研究成果于12月17日在线发表在《高级材料》杂志上。
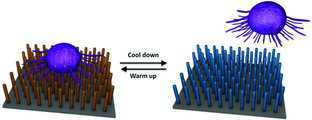
类似的细胞捕捉设备已经有过报道,但这项技术的独特之处在于,它能够以极高的效率捕捉到肿瘤细胞和随后释放出具有优良活力的肿瘤细胞。该设备就像一个过滤器,它包含一种结构像尼龙搭扣样的颗粒,血液通过后够吸附和分离肿瘤细胞,效率介于40%到70%之间。
“迄今为止,已有数种设备能够以高效率捕获循环肿瘤细胞,可是,为了获得更有意义的信息,释放、保存和研究这些细胞也同样的重要。这就是我们的设备与众不同的地方”,负责领导团队发明覆盖于该设备的聚合物刷的Hsiao-hua Yu解释道。
与癌细胞相关的拓展阅读:
- 红外线照射碳纳米管杀死癌细胞
- 按捏乳房可抑制乳腺癌细胞生长
- 自主发光蛋白标识癌细胞
- AM J RESP CRIT CARE:Th9细胞对肺癌细胞的免疫调节
- Nat Commun:粘附分子帮助癌细胞挣脱原位转移至新组织 更多信息请点击:有关癌细胞更多资讯

DOI: 10.1002/adma.201203185
PMC:
PMID:
Capture and Stimulated Release of Circulating Tumor Cells on Polymer-Grafted Silicon Nanostructures
Shuang Hou1,†, Haichao Zhao2,†, Libo Zhao1,Qinglin Shen1,4, Kevin S. Wei1, Daniel Y. Suh1,Aiko Nakao3, Mitch A. Garcia1, Min Song1, Tom Lee1, Bin Xiong4, Shyh-Chyang Luo2,*, Hsian-Rong Tseng1,*, Hsiao-hua Yu2,*
A platform for capture and release of circulating tumor cells is demonstrated by utilizing polymer grafted silicon nanowires. In this platform, integration of ligand-receptor recognition, nanostructure amplification, and thermal responsive polymers enables a highly efficient and selective capture of cancer cells. Subsequently, these captured cells are released upon a physical stimulation with outstanding cell viability.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Advanced#
67
#新技术#
60
#血液循环#
78
#癌细胞#
88