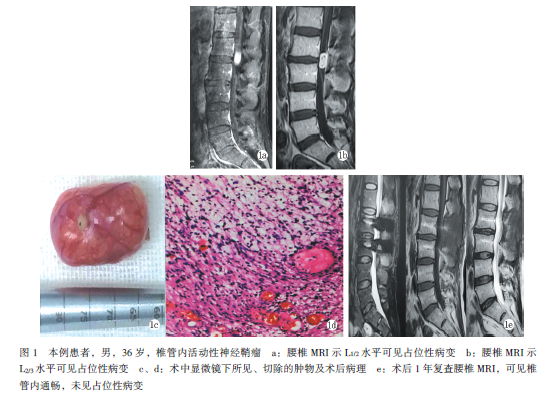
腰椎椎管内可活动性神经鞘瘤1例
2019-09-04 邵元栋 于益民 中国矫形外科杂志
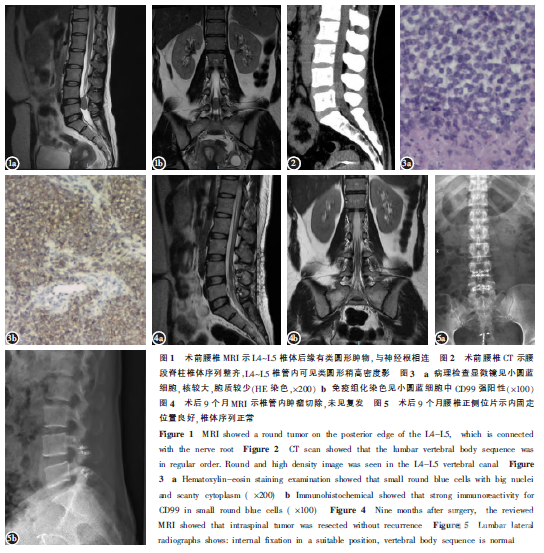
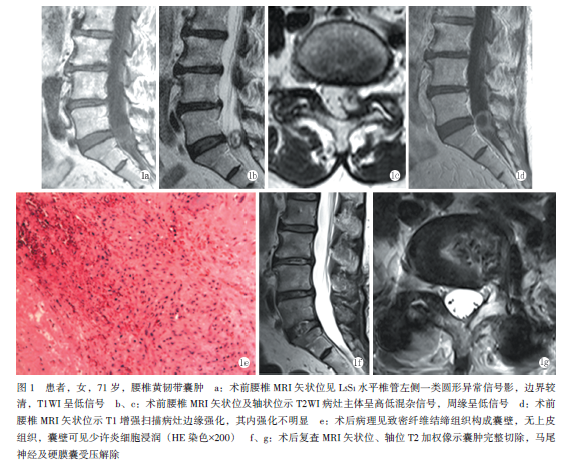
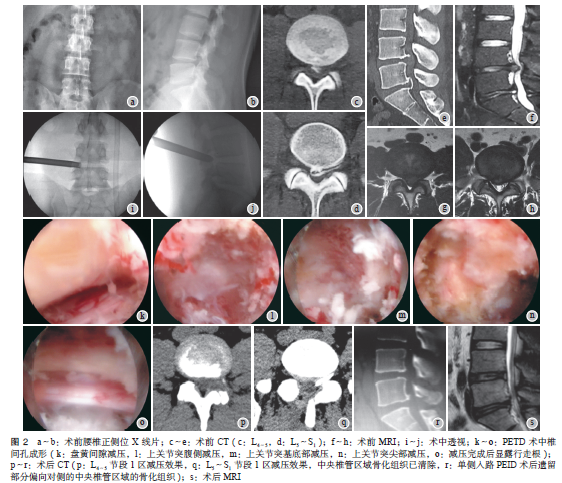
椎管内神经鞘瘤是最常见的椎管内良性肿瘤,约占椎管内良性肿瘤一半,其起源于神经根的鞘膜,大部分位于髓外硬脊膜下间隙。大部分起源于脊神经后根,受累神经呈纺锤状,一般单发。临床中一旦确诊均应手术治疗。手术方法以后入路椎板切除最为常见。2017年7月,作者对1例椎管内神经鞘瘤行手术治疗,发现术前MRI检查与术中肿瘤实际位置不一致,现报告如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#活动性#
62
#椎管内#
72
#椎管#
80
#腰椎#
59
#神经鞘瘤#
72