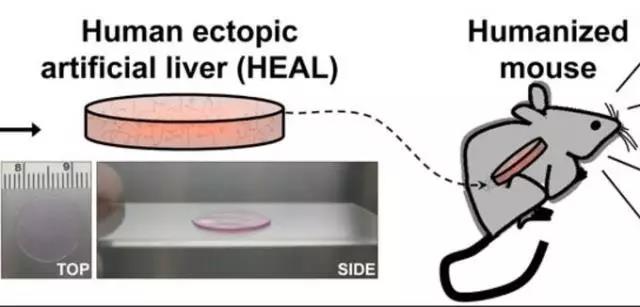
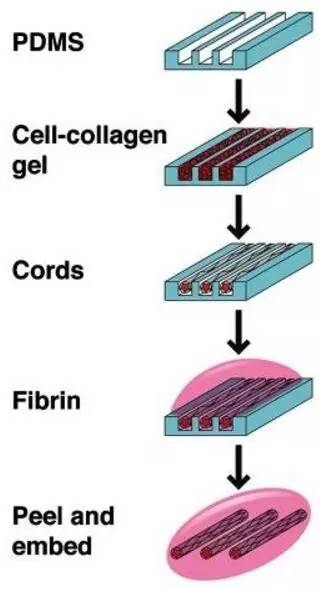
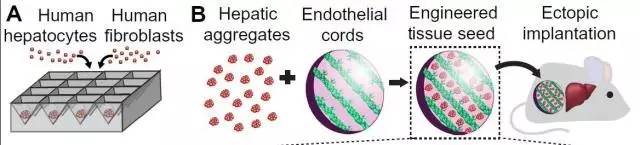
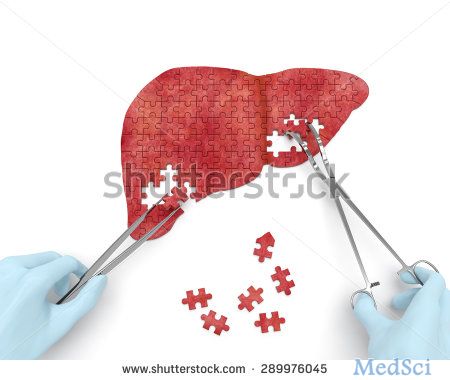
Sci Transl Med:振奋人心!MIT科学家「种植」迷你肝,成功扩大50倍,长成具有主要功能的肝脏
2017-07-30 王鑫英 奇点网
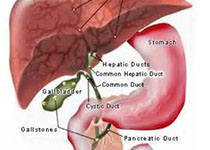
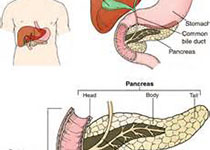
慢性肝炎会带来很高的肝硬化和肝癌风险,可能会引起过早死亡。针对终末期肝病,唯一有效的治疗就是肝移植。然而,2009年资料显示,我国肝受体和肝供体的比例接近100:1[1],即大约100个需要肝移植的患者去争夺1个捐献的肝脏!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Transl#
48
#TRA#
57
#MIT#
70
#种植#
55
#Med#
71
学习了,谢谢分享!
80
henhao
85