FTD(TAS-102)后线治疗晚期胃癌疗效与安全性并优
2019-06-11 复旦大学附属肿瘤医院朱晓东教授 肿瘤资讯
TFTD(研发代号:TAS-102)是一种新型的口服细胞毒抗肿瘤药物,目前已在全球60多个国家和地区获批用于转移性结直肠癌(mCRC)后线治疗。与转移性结直肠癌后线治疗一样,转移性胃癌后线治疗药物也十分匮乏。因此开展了TAGS研究,探索TFTD对转移性胃或胃食管结合部(GEJ)腺癌(mGC/mGEJC)的疗效和安全性。这是一项随机、双盲、安慰剂对照Ⅲ期研究,在17个国家的110家医院开展。TAGS
TFTD(研发代号:TAS-102)是一种新型的口服细胞毒抗肿瘤药物,目前已在全球60多个国家和地区获批用于转移性结直肠癌(mCRC)后线治疗。与转移性结直肠癌后线治疗一样,转移性胃癌后线治疗药物也十分匮乏。因此开展了TAGS研究,探索TFTD对转移性胃或胃食管结合部(GEJ)腺癌(mGC/mGEJC)的疗效和安全性。这是一项随机、双盲、安慰剂对照Ⅲ期研究,在17个国家的110家医院开展。TAGS研究入组既往接受≥2线化疗的转移性胃及胃食管交界部腺癌患者,按2︰1随机分配至TFTD组(N=337例)或安慰剂组(N=170例)。主要研究终点是总生存期(OS),结果TFTD组的中位OS显着高于安慰剂组(5.7 vs 3.6个月),HR 0.69; P=0.00029。2018年10月,TAGS全文发表于国际权威期刊《柳叶刀肿瘤》。基于TAGS研究令人振奋的结果,2019年2月,FDA批准TFTD用于既往接受过至少2线化疗的转移性胃或胃食管结合部(GEJ)腺癌的治疗,且2019年版美国国立综合癌症网络(NCCN)胃癌临床实践指南将TFTD列为转移性胃癌后线治疗的标准方案。
2019年ASCO:TFTD四项分析研究结果齐亮相
在今年的ASCO年会上,有4项TAGS相关研究亮相,分别从生活质量、高龄亚组及胃食管交界部腺癌亚组对TAGS研究结果进行了深度剖析,此外还汇总分析了TFTD在RECOURSE研究和TAGS研究中的安全性数据。
Abs4043. TFTD能很好地维持mGC/mGEJC患者的生活质量
分别在基线和每间隔4周采用EORTC QLQ-C30和QLQ-ST022量表对TAGS研究的两组患者进行生活质量评估。TFTD组和安慰剂组分别有98.5%和96.5%的患者完成了基线的QoL评估,两组患者基线的QoL评分大体相似。通过对死亡和进展事件的敏感性分析显示,TFTD相比于安慰剂可以降低QoL各个项目恶化的风险(HRs范围为0.57~0.74),很好地维持了mGC/mGEJC患者的生活质量。
Abs4037. TFTD对高龄患者(≥65岁)安全有效
TAGS研究纳入了228例(45%)年龄≥65岁(范围65~89岁)的患者,同总人群相比,高龄患者基线中度肾功能损伤比率更高(31% vs 17%)。高龄亚组中TFTD组基线ECOG评分更差些(TFTD组同安慰剂组ECOG 1的患者占比为69% vs 59%)。结果高龄亚组患者中,TFTD显示了和总体人群中一致的生存优势,同安慰剂组比中位OS分别为6.2和5.4个月,HR 0.73(0.52~1.02)。AE分析结果高龄亚组同总人群中基本一致。这一结果证实,即使在中度肾功能损害发生率较高的高龄(≥65岁)患者中,TFTD仍然安全有效,且对轻中度肾功能损害的患者,初始给药无需调整剂量。
Abs4038. TFTD对mGEJC患者安全有效
TAGS研究中有145例(29%)mGEJC患者(TFTD组 98例 vs 安慰剂组 47例)。与安慰剂组相比,TFTD组既往接受过胃切除术的患者比例更低(40% vs 55%),接受过≥3线治疗的患者比例更高(74% vs 66%)。疗效分析显示,TFTD和安慰剂组的中位OS分别为4.8个月和3.5个月,HR为0.75(0.50~1.11)。这一研究结果证实,即使TFTD组患者既往接受过更多线的治疗,对于mGEJC患者仍显示出良好的安全性和疗效。
Abs4039. TFTD在mGC/mGEJC和mCRC中显示出一致的安全性及耐受性
基于Ⅲ期RECOURSE和TAGS研究结果,TFTD分别获批用于经治转移性结直肠癌(mCRC)和mGC/mGEJC。两个研究中TFTD的安全性相似,TFTD组最常见的≥3级不良事件如:中性粒细胞降低(在TAGS和RECOURSE两个研究中的发生率分别为34%和35%)、贫血(19%和17%)和白细胞降低(9%和13%);对比分析显示:TFTD在mGC/mGEJC和mCRC中显示出一致的安全性及耐受性。
总结
创新药物的不断涌现在各癌种治疗领域展露锋芒、势不可挡,但在胃癌领域的探索却是另一番境地,靶向治疗举步维艰,免疫治疗曙光初现,似乎说明全身系统化疗仍是胃癌治疗的基石。
TAGS研究在转移性胃癌领域取得的突破及一系列分析研究证实了TFTD对mGC患者安全有效,且能很好的维持患者的生活质量,为转移性胃癌后线治疗增添了有价值的临床治疗选择。
TFTD:研发代号TAS-102,又称FTD/TPI,由三氟胸苷(FTD)和盐酸替匹嘧啶(TPI)以1:0.5的摩尔比组合而成。TFTD的主要作用机制是FTD在DNA复制的过程中取代胸腺嘧啶掺入DNA双链,导致DNA功能障碍发挥抗肿瘤作用;同时TPI可以抑制胸苷磷酸化酶(TPase)活性,抵抗氟嘧啶耐药。
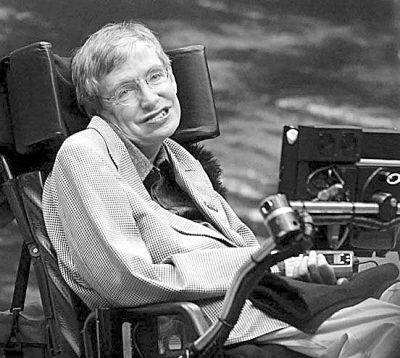
朱晓东教授,复旦大学附属肿瘤医院肿瘤内科主任医师,硕士研究生导师,中国抗癌协会肿瘤临床化疗专业委员会青年委员会委员,中国宋庆龄基金会肿瘤医疗及产学研联盟理事,中国抗癌协会肿瘤营养与支持治疗专业委员会肿瘤营养化疗学组委员,中国医药教育协会腹部肿瘤专业委员会委员,上海市抗癌协会胃肠肿瘤专业委员会委员,上海市抗癌协会癌症康复与姑息治疗专业委员会(CRPC)委员,Focus on Gastrointestinal Tumors杂志Editorial Board member
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TAS-102#
56
#疗效与安全性#
61
#晚期胃癌#
57
#S-1#
67
#FTD#
77
谢谢梅斯提供这么好的信息,学到很多
76