ESO:tPA用于严重卒中患者安全
2015-05-06 佚名 医学论坛网
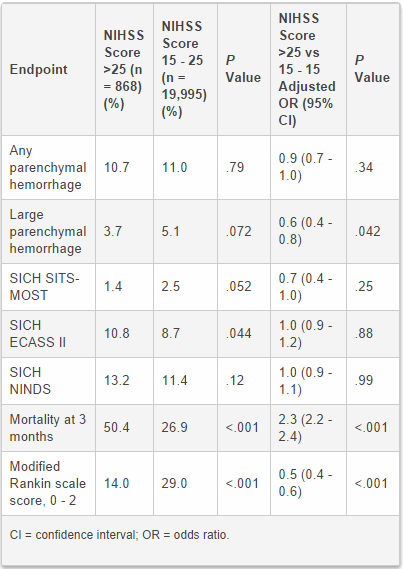
一项来自溶栓治疗中风的大型国际注册新数据表明,组织型纤溶酶原激活剂(tPA,阿替普酶)用于严重卒中患者具有安全性。 “我们未发现严重卒中患者应用后存在出血风险,美国国立卫生院中风量表NIHSS对其评分超过25分。”该研究的第一作者、来自瑞典斯德哥尔摩卡罗林斯卡医学院的Michael Mazya博士总结道。他在2015年首届欧洲脑卒中大
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#卒中患者#
59
#患者安全#
58
#tPA#
91
#ESO#
65
看过了
202
看看
153
不错……
138
很好,学习了!
158
以后可以放心使用了!
92