IBD:轻微便血可以减少炎症性肠病患者静脉血栓栓塞的发生
2020-09-03 MedSci原创 MedSci原创
有研究已经证实,住院的炎症性肠病(IBD)患者的静脉血栓栓塞(VTE)风险要高3倍,而当IBD患者因活动性疾病住院时,该风险增加到6倍。
有研究已经证实,住院的炎症性肠病(IBD)患者的静脉血栓栓塞(VTE)风险要高3倍,而当IBD患者因活动性疾病住院时,该风险增加到6倍。为了降低住院IBD患者的VTE风险,目前多指南均建议对患有严重疾病但没有严重出血的溃疡性结肠炎(UC)患者使用药物预防VTE的发生。本项研究旨在探究影响VTE的危险因素究竟有哪些。

研究人员对2013年1月至2018年8月期间住院的IBD患者进行了回顾性队列研究。主要结果是预防VTE措施的实施,关注的暴露范围包括急性和慢性出血。
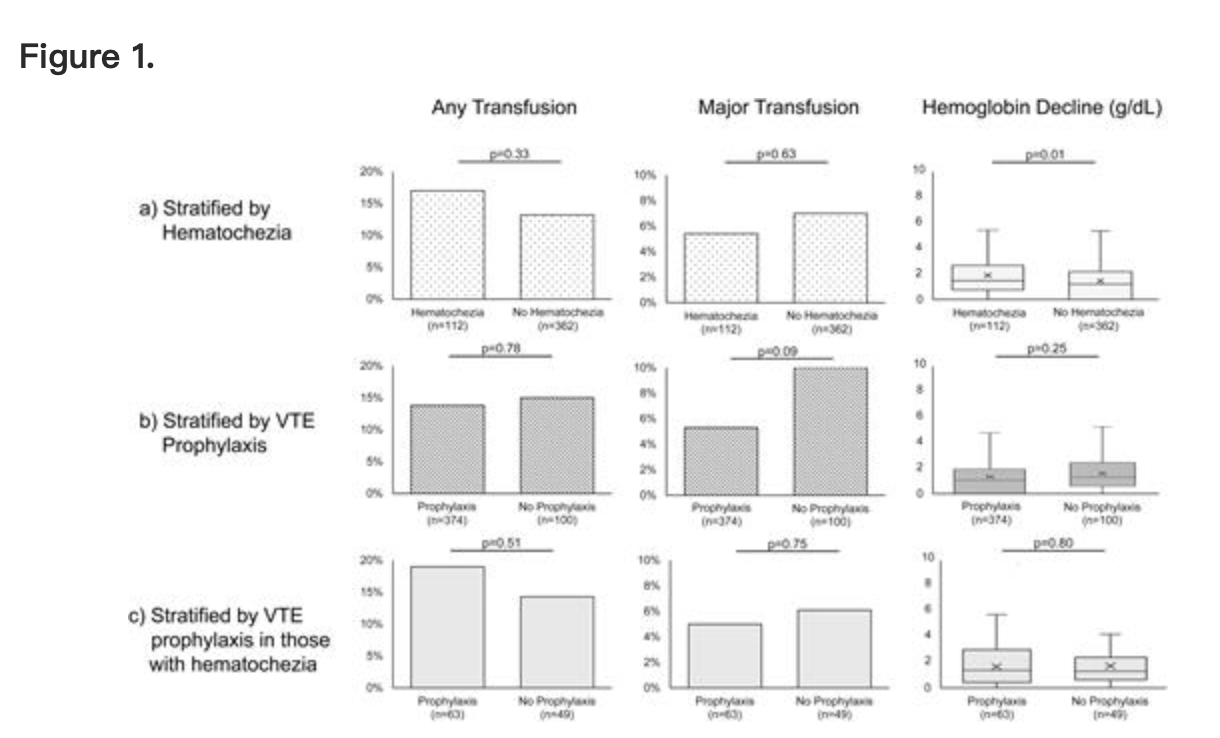
本项研究共纳入了22499名患者,其中474名(2%)IBD。IBD患者不太可能接受VTE预防(IBD患者为79%,非IBD患者为87%),特别是如果存在便血(便血患者为57%,非便血患者为86%)。在IBD患者中,入院和便血(调整后的优势比为0.27; 95%CI为0.16-0.46)是减少VTE预防使用的最强独立预测指标。预防出血和静脉血栓栓塞均与住院期间输血率增加或血红蛋白水平临床上显着下降无关。
因此,如果住院的患者患有IBD,则不太可能接受VTE预防,而便血可能会导致这种情况更加经常的出现。
原始出处:
Adam S Faye. Et al. Minor Hematochezia Decreases Use of Venous Thromboembolism Prophylaxis in Patients with Inflammatory Bowel Disease. Inflammatory Bowel Diseases.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉血#
81
#静脉#
0
#IBD#
108
#便血#
94
#炎症性#
83
#炎症性肠病患者#
71