上海第九人民医院静脉曲张专科
2016-08-23 MedSci MedSci原创
在我国,下肢静脉曲张的发病率很高,是血管外科的常见疾病,可引发皮肤瘙痒、色素沉着,进而造成溃疡及出血,严重影响着人们的身体健康和生活质量。我国约有1亿多人患有不同程度的下肢静脉曲张。近年来静脉曲张的发病率逐年上升,发病人群有年轻化的趋势,现在门诊经常见到20多岁就得静脉曲张的就诊者,因此各个年龄阶段的人都不能轻视静脉曲张。 上海交通大学医学院附属第九人民医院血管外科成立于上世纪80年代,在国内享有
在我国,下肢静脉曲张的发病率很高,是血管外科的常见疾病,可引发皮肤瘙痒、色素沉着,进而造成溃疡及出血,严重影响着人们的身体健康和生活质量。我国约有1亿多人患有不同程度的下肢静脉曲张。近年来静脉曲张的发病率逐年上升,发病人群有年轻化的趋势,现在门诊经常见到20多岁就得静脉曲张的就诊者,因此各个年龄阶段的人都不能轻视静脉曲张。
上海交通大学医学院附属第九人民医院血管外科成立于上世纪80年代,在国内享有极高声誉。静脉曲张专科是第九人民医院的特色专科,在下肢静脉曲张的微创治疗方面处于国内领先地位,也 是全国首批VDM(Venous DiseaseMedical Center)治疗中心。
传统的静脉曲张手术是抽剥大隐静脉主干同时对小腿曲张静脉做多切口剥离,这种手术方式切口长,创伤大,术后皮肤残留许多瘢痕,极大影响了皮肤的美观。九院的静脉曲张专科是国内最早开展静脉曲张腔内激光微创治疗和硬化剂注射治疗的单位之一。我们对静脉曲张患者采用个体化多普勒超声进行精确术前定位,采用硬化剂注射治疗及腔内激光治疗,下肢静脉曲张的病人在术后当日就可以下地行走,并离院回家,真正做到了微创、便捷、安全。
另外,夏季一到,爱美的女士们都换上了清凉的夏装,可是,许多姑娘们却终日长裙长裤,为什么呢?原因就是她们腿部的红血丝,许多爱美的女士常常为此十分困扰。现在女士们越来越注意自己的形象及生活质量,对毛细血管扩张治疗的需求也越来越大。下肢毛细血管扩张的治疗是我们的一大治疗特色,许多女性患者治疗后终于敢秀出了美腿。
静脉期曲张日间手术流程
手术当日抵达医院
激光联合硬化剂微创手术
仅需术中局部麻醉
患者全程清醒、舒适
术中超声实时定位、全程监测
术后30分钟即可步行回家

当日医生接诊登记

术前沟通、签署知情同意书

术前超声定位并描记

术前准备完毕、心电监护实时监测
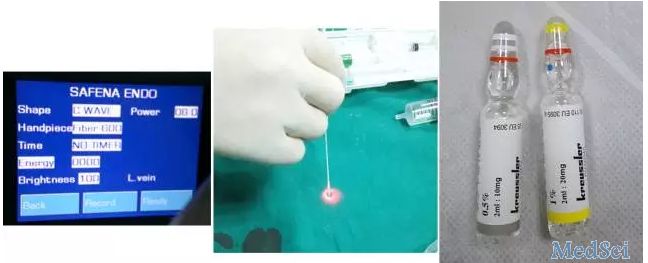
环形激光及硬化剂

麻醉

置入光纤

超声下监测治疗

硬化剂注射
局部麻醉并激光、硬化剂治疗


术毕腿部美观、无明显创面
观察患者30分钟无明显不适,患者步行离院
术后随访恢复良好,患者满意
陆信武教授
上海交通大学附属第九人民医院血管外科主任,擅长血管外科各类疾病的诊断和治疗,首创累及弓上分支的主动脉疾病的激光原位开窗技术,开辟了主动脉疾病治疗的新领域。近年来以第一申请人和主要实施者承担国家自然基金项目等8项课题,以第一作者在国内外杂志上发表论文75篇,获多项临床科技成果奖。教育部科技奖励评审专家,国家自然资金一审专家及多本杂志编委和审稿人。
赵海光,外科学博士,上海交通大学附属第九人民医院血管外科静脉曲张专科主诊医师。国际血管联盟中国分会青年委员、中国医师协会先天性脉管畸形专委会委员、中国整形美容协会激光美容分会青年委员、中国整形美容协会瘢痕医学分会青年常委、上海市中医药学会周围血管病专业委员会副主任委员。从事血管外科疾病临床诊疗工作10余年,经验丰富,尤其在下肢静脉曲张、毛细血管扩张、血管畸形的微创治疗和皮肤激光美容方面有较深的造诣。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉#
61
#人民医院#
73
#专科#
71
很好,不错,以后会多学习
170