Int J Clin Pharm:术后患者静脉血栓栓塞的风险因素
2017-05-15 门鹏;常路 环球医学
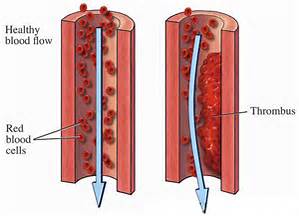
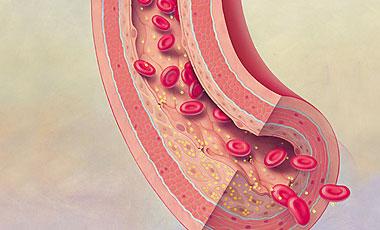
手术后,患者处于较高的进展静脉血栓栓塞症的风险,临床表现为深静脉血栓(DVT)或肺栓塞(PE)。2017年4月,发表在《Int J Clin Pharm.》的一项病例对照研究表明,多药治疗和血液产品是术后患者静脉血栓栓塞的风险因素。
手术后,患者处于较高的进展静脉血栓栓塞症的风险,临床表现为深静脉血栓(DVT)或肺栓塞(PE)。2017年4月,发表在《Int J Clin Pharm.》的一项病例对照研究表明,多药治疗和血液产品是术后患者静脉血栓栓塞的风险因素。
目的:旨在评估多药治疗、合并症、药物治疗、红细胞输血、预防血栓形成的充分性、患者特征等,对术后患者DVT或PE发生率的影响。
设置:斯洛文尼亚穆尔斯卡索博塔总医院外科。
方法:在这项回顾性病例对照研究中,分析了286例手术患者记录:DVT或PE组(144人)和对照组(142人)。研究人员审查了处方药物的数量和药物-药物相互作用,以及低分子量肝素的处方。DVT或PE风险因素的比值比(OR)使用多变量逻辑回归模型进行计算。
主要结局测量:手术患者DVT或PE复发风险因素的评估。
结果:多药治疗(OR,2.02;95% CI,1.03~3.96;P=0.040)和红细胞输血(OR,3.44;95% CI,1.46~8.10;P=0.005)与术后PE或DVT风险的增加相关。使用低分子量肝素进行充分的预防血栓形成会显著增加DVT或PE的可能性(OR,2.50;95% CI,1.41~4.43;P=0.002)。在涉及非甾体抗炎药、苯二氮卓类药物或抗精神病药治疗上,组间没有差异。
结论:多药治疗的患者和接受红细胞输血的患者术后应该密切监测,这是由于他们很可能发生DVT或PE。
原始出处:
Premuš Marušič A, et al.Polypharmacotherapy and blood products as risk factors for venous thromboembolism in postsurgical patients: a case-control study. Int J Clin Pharm. 2017 Apr;39(2):416-423. doi: 10.1007/s11096-017-0441-7.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#静脉#
53
#静脉血#
53
#Pharm#
51
继续学习
78
学习了,分享了
79
学习啦,谢谢分享
73
患者术后活动是“受限,静脉血流缓慢引起血栓
62
学习一下谢谢分享
73
学习一下
42