JCI:中山大学潘景轩教授找到可能彻底治愈常见白血病的新靶点
2016-09-22 佚名 生物谷
近日,来自中国中山大学的潘景轩教授带领研究团队在慢性髓性白血病(CML)的治疗靶点开发方面取得重要进展,他们发现甲基转移酶PRMT5是维持白血病干细胞存活和自我更新的重要因子,该研究成果有望推动对CML彻底治愈的进程。 对CML治疗药物伊马替尼不敏感的白血病干细胞被认为是CML抵抗BCR-ABL酪氨酸激酶抑制剂以及出现疾病复发的主要原因。发现新治疗靶点,清除白血病干细胞可能是治愈CML的一种

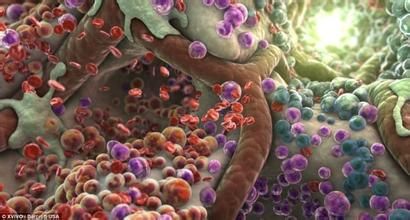
近日,来自中国中山大学的潘景轩教授带领研究团队在慢性髓性白血病(CML)的治疗靶点开发方面取得重要进展,他们发现甲基转移酶PRMT5是维持白血病干细胞存活和自我更新的重要因子,该研究成果有望推动对CML彻底治愈的进程。
对CML治疗药物伊马替尼不敏感的白血病干细胞被认为是CML抵抗BCR-ABL酪氨酸激酶抑制剂以及出现疾病复发的主要原因。发现新治疗靶点,清除白血病干细胞可能是治愈CML的一种策略。
在这项研究中,研究人员在CML细胞中发现BCR-ABL和蛋白质精氨酸甲基转移酶5(PRMT5)之间存在一个正反馈回路。他们观察到人类CML白血病干细胞中存在PRMT5过表达的现象。之后研究人员利用shRNA对PRMT5的基因表达进行沉默,也利用小分子抑制剂PJ-68阻断PRMT5的甲基转移酶活性,均发现能够降低来自CML病人的白血病干细胞的存活,抑制长期培养起始细胞。
更进一步的研究表明,降低PRMT5表达或用抑制剂抑制其活性能够显著延长CML小鼠模型的生存时间,损伤移植到体内的CML白血病干细胞在体内的自我更新能力。除此之外PJ-68还会抑制人类CML CD34+细胞在免疫缺陷小鼠体内的长期移植效果。研究人员还发现抑制PRMT5能够通过减少DVL3蛋白干扰Wnt/b-catenin信号途径在CML CD34+细胞中的作用。
这项研究表明对组蛋白精氨酸残基的甲基化修饰是控制白血病干细胞自我更新的一种可调控机制,因此PRMT5有望成为对抗白血病干细胞的一个潜在治疗靶点。
原始出处
Yanli Jin,1 Jingfeng Zhou,1 Fang Xu,1 Bei Jin,1 Lijing Cui,2 Yun Wang,1 Xin Du,3 Juan Li,4 Peng Li,5 Ruibao Ren,6 and Jingxuan Pan.Targeting methyltransferase PRMT5 eliminates leukemia stem cells in chronic myelogenous leukemia.JCI.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCI#
71
太棒了
110
太好了!
111
#新靶点#
58
#中山大学#
62
好牛逼~~~~~~
106
到临床还有一段距离!!!
105
不错,一大突破!恭喜科研
101
继续关注!
105
谢谢分享!
68