Lancet Oncol:化疗与厄洛替尼交替可使NSCLC患者受益(FASTACT-2研究)
2013-07-13 MedSci MedSci原创
广东省人民医院吴一龙教授等开展的FASTACT-2研究最新结果显示,化疗与厄洛替尼交替治疗方案可显著延长晚期非小细胞肺癌(NSCLC)患者的无进展生存期(PFS)和总生存期(OS),EGFR基因突变患者获益明显。(Lancet Oncology.2013年6月17日在线版)。 FASTACT研究为一项随机、安慰剂对照临床研究。在2009年4月29日~2010年9月9日的Ⅲ期研究中,研究者入选
广东省人民医院吴一龙教授等开展的FASTACT-2研究最新结果显示,化疗与厄洛替尼交替治疗方案可显著延长晚期非小细胞肺癌(NSCLC)患者的无进展生存期(PFS)和总生存期(OS),EGFR基因突变患者获益明显。(Lancet Oncology.2013年6月17日在线版)。
FASTACT研究为一项随机、安慰剂对照临床研究。在2009年4月29日~2010年9月9日的Ⅲ期研究中,研究者入选451例从未接受治疗的ⅢB或Ⅳ期非小细胞肺癌患者,根据病情分期、肿瘤组织结果、吸烟状态及化疗方案等,将患者按1:1的比例,每4周接受6个周期的吉西他滨(1250mg/m2,第1d和第8d,静脉注射)及铂制剂(卡铂5×曲线下面积或顺铂75mg/m2,第1d,静脉注射)治疗,随机联合厄洛替尼(150mg/d,第15~28d,口服;化疗联合厄洛替尼)或安慰剂口服治疗。安慰剂组患者若出现病情进展,接受厄洛替尼二线治疗。
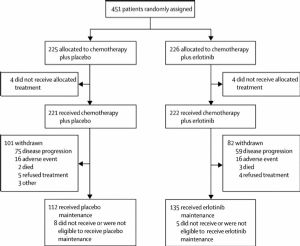
Figure1 Trial
profileChemotherapy=gemcitabine plus carboplatin or cisplatin.
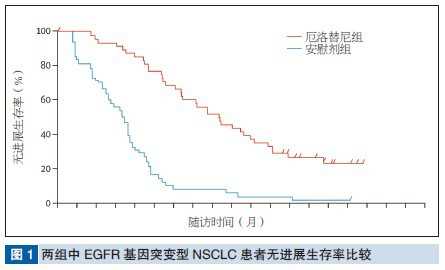
结果显示,厄洛替尼组患者的PFS显著长于安慰剂组患者,两组的中位PFS分别为7.6个月和6.0个月(HR=0.57,P<0.0001);厄洛替尼组的中位OS也比安慰剂组要长(18.3个月与15.2个月(HR=0.79,P=0.042)。研究发现,仅存在活化表皮生长因子受体(EGFR)基因突变的患者从化疗和厄洛替尼交替治疗中得到生存获益,其中位PFS(16.8个月与6.9个月,HR=0.25,P<0.0001,图1)和OS(31.4个月与20.6个月,HR=0.48,P=0.0092)均较安慰剂组显著延长。安慰剂组和厄洛替尼组的严重不良事件发生率分别为34%和31%,最常见的3级或以上级别不良事件为中性粒细胞减少(29%与25%)、血小板减少(14%与14%)和贫血(12%与9%)。
研究者观点
IPASS、First-SIGNAL、NEJ、WJTOG、OPTIMAL和EURTAC6等Ⅲ期临床研究提示,NSCLC患者接受EGFR-酪氨酸激酶抑制剂单独治疗无OS获益。既往几项临床随机研究已表明,化疗和EGFR-酪氨酸激酶抑制剂交替治疗对NSCLC患者有益。该随机Ⅲ期临床研究首次显示,化疗和EGFR抑制剂交替治疗可提高EGFR基因突型晚期NSCLC患者的PFS和OS。
在中国,EGFR基因检测率并不高,尽管化疗与厄洛替尼交替治疗对EGFR基因突变型患者疗效更佳,但对无EGFR基因突变的患者也无害处。对于该类患者,化疗和厄洛替尼交替治疗方案疗效很有可能优于标准化疗。因此,对于EGFR突变状态不明但临床指标高度提示为EGFR突变的NSCLC患者,化疗与厄洛替尼交替治疗也是一种可行的一线治疗手段。
原始出处:
Wu YL, Lee JS, Thongprasert S, Yu CJ, Zhang L, Ladrera G, Srimuninnimit V, Sriuranpong V, Sandoval-Tan J, Zhu Y, Liao M, Zhou C, Pan H, Lee V, Chen YM, Sun Y, Margono B, Fuerte F, Chang GC, Seetalarom K, Wang J, Cheng A, Syahruddin E, Qian X, Ho J, Kurnianda J, Liu HE, Jin K, Truman M, Bara I, Mok T.Intercalated combination of chemotherapy and erlotinib for patients with advanced stage non-small-cell lung cancer (FASTACT-2): a randomised, double-blind trial. Lancet Oncol. 2013 Jul;14(8):777-86.
PDF全文下载:![]() s1470204513702547.pdf
s1470204513702547.pdf
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Lancet#
51
#FAST#
66
#Oncol#
46
#FAS#
51
#SCLC患者#
0
#TAC#
58
#AST#
44
#厄洛替尼#
50
#NSCLC患者#
58