Phytomedicine:茯苓提取物通过调节脑肠肽、免疫、修复胃肠粘膜改善功能性消化不良
2021-12-18 Vivi MedSci原创
探讨茯苓及其三种提取物(三萜类,PCT;水溶性多糖,PCWP;酸性多糖,PCAP)对大鼠FD的治疗作用及其作用机制,以探索PC提取物治疗FD的活性物质,充分利用其医学价值。
背景:茯苓在中国被用作食品和药物已有2000多年的历史,对功能性消化不良(FD)有很好的治疗效果。但其物质基础和作用机制尚未见报道。
目的:探讨茯苓及其三种提取物(三萜类,PCT;水溶性多糖,PCWP;酸性多糖,PCAP)对大鼠FD的治疗作用及其作用机制,以探索PC提取物治疗FD的活性物质,充分利用其医学价值。
方法:采用超高效液相色谱四极杆串联飞行时间质谱联用(UPLC-Q-TOF-MS)和凝胶渗透色谱(GPC/SEC)对PC提取物的化学成分进行分析和定量。采用负重强迫游泳和隔日禁食42 d的方法建立FD大鼠模型,70只Wistar大鼠分为对照组、模型组、补中益气丸组、PCD组(茯苓水煎剂)、PCT组、PCWP组、PCAP组。治疗14天后,采用ELISA、组织病理学、免疫组织化学和Western blot等方法观察其作用及机制。
结果:共鉴定出77种三萜类化合物。PCWP主要由A组分(Mw: 3.831 ×107 Da)、B组分(Mw: 5.650 ×106 Da)和C组分(Mw: 113117 Da)组成。PCAP为均一组分,平均分子量为74320 Da。
PCT、PCWP和PCAP均能缓解FD症状。与对照组相比,模型组大鼠心、肾、肝、肺、胃和小肠脏器指数差异无统计学意义,脾脏和胸腺指数显著降低。与模型组相比,BZYQP、PCD和PCAP组血清D-xylose、ACh、ALB和TP水平均显著或极显著升高。
与模型组相比,PCD、PCT和PCWP显著提高GAS水平,BZYQP和PCD显著提高MTL水平,BZYQP、PCD和PCWP显著提高VIP水平,BZYQP、PCD、PCT和PCWP显著降低CCKAR和CGRP水平,显著提高SP水平,各提取物均能降低5-HT水平。免疫组织化学染色和Western blotting检测胃饥饿素在胃组织中的表达情况,PCD、PCT和PCAP均能增加胃饥饿素的表达。这些结果表明PC通过调节脑肠肽改善FD。
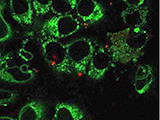
模型组大鼠胃和小肠组织的H&E染色显示胃上皮细胞坏死,脱落进入胃腔。肠上皮细胞坏死脱落进入肠腔,肠绒毛被破坏。在所有剂量组中,这些病理体征均显著改善。MUC2黏液可形成一个物理屏障,防止肠道微生物成分进入宿主。EGF和EGFR在胃粘膜的再生过程中发挥重要作用。免疫组织化学检测EGFR和MUC2,ELISA检测血清EGF。BZYQP、PCD、PCT和PCAP组胃EGFR表达水平显著升高,血清EGF水平在所有剂量组均显著升高,各剂量组肠道MUC2表达水平均显著升高。AQPs在胃生理中的功能可能涉及水转移及屏障功能,在PCT、PCWP和PCAP组胃AQP1表达显著下降。以上结果表明PC通过促进胃肠粘膜的修复改善FD。
FD与机体免疫相关,故检测相关免疫细胞因子和蛋白水平(TGF-β1, IL-1β, IL-2, IL-4, IL-6, IL-17, IFN-γ, TNF-α),结果表明PC通过提高免疫力改善FD。TLR和JNK信号通路在免疫和炎症中发挥着重要作用,TRAF6和c-Jun分别是这两种信号通路中的关键转录因子。免疫组化和WB结果显示p-c-Jun在PCD、PCT、PCWP和PCAP组表达下降,TRAF6在PCD、PCT、PCWP和PCAP组表达下降。
结论:PC提取物对FD大鼠有一定的治疗作用,其作用机制涉及多种途径。在传统应用中经常被忽略的PCAP是有效的。该研究为PC提取物的应用和开发提供了新的思路。
文献来源:
Tu, Y., Luo, X., Liu, D., et al. (2021). Extracts of Poria cocos improve functional dyspepsia via regulating brain-gut peptides, immunity and repairing of gastrointestinal mucosa. Phytomedicine : international journal of phytotherapy and phytopharmacology, 95, 153875. Advance online publication. https://doi.org/10.1016/j.phymed.2021.153875
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了,是一个艰难的过程,为你们点赞。
86
#CIN#
69
#粘膜#
80
#DIC#
71
#功能性#
89
#Medicine#
56
#Med#
70