Eur Heart J:病因不明的房室传导阻滞年轻患者长期结局
2021-02-21 MedSci原创 MedSci原创
在50岁之前出现并经起搏器植入治疗的病因不明AVB与因心衰、室性心律失常或复苏成功的心脏骤停而死亡或住院的综合终点发生率增加三到四倍相关。持续性AVB患者的风险较高。
年轻人中病因不明的房室传导阻滞(AVB)很少见,这些患者的结局也尚未明确。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在评估病因不明的AVB年轻患者长期发病率和死亡率。
研究人员确定了1996年1月至2015年12月期间丹麦所有接受起搏器治疗年龄小于50岁的AVB患者。研究人员通过回顾病历,纳入了病因不明的AVB患者,并组建了匹配的对照队列。研究人员通过国家登记机构进行了随访。该研究的主要结局包括死亡、心衰住院、室性心律失常和成功复苏的心脏骤停在内的综合终点。
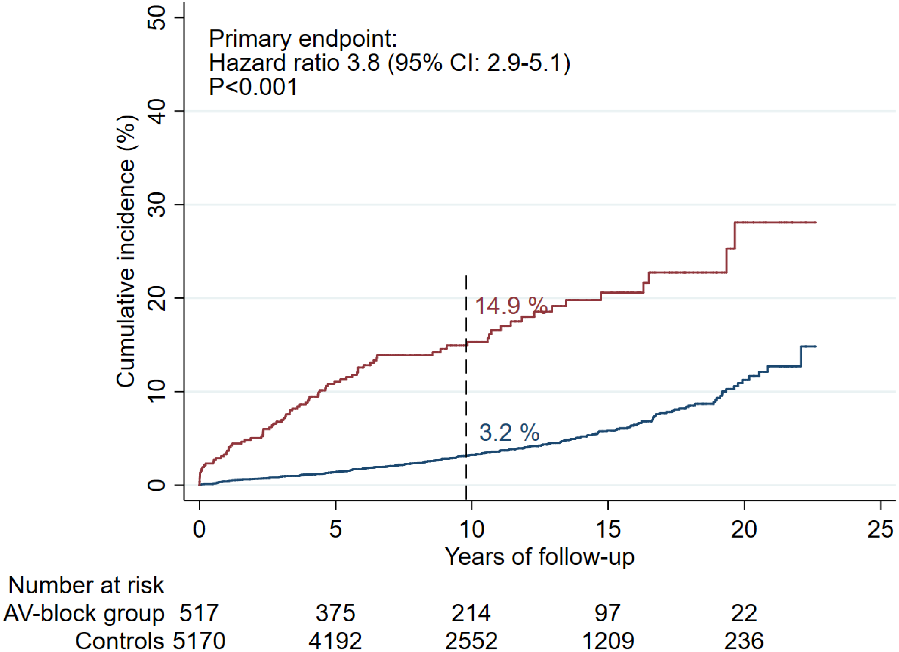
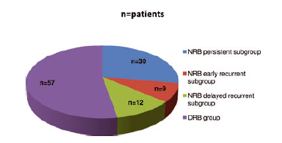
研究人员纳入了517例患者和5170例对照者,首次植入起搏器的中位年龄为41.3岁[四分位间距(IQR)为32.7-46.2岁]。在中位随访9.8年(IQR为5.7–14.5年)后,14.9%的患者和3.2%的对照者发生了主要终点[风险比(HR)为3.8;95%置信区间(CI)为2.9-5.1;P<0.001]。持续性AVB患者在确诊时的主要终点风险较高(HR为10.6;95%CI为5.7-20.0;P<0.001),且在随访早期风险最高(在随访的0–5年内HR为6.8;95%CI为4.6-10.0;P<0.001)。
由此可见,在50岁之前出现并经起搏器植入治疗的病因不明AVB与因心衰、室性心律失常或复苏成功的心脏骤停而死亡或住院的综合终点发生率增加三到四倍相关。持续性AVB患者的风险较高。
原始出处:
Johnni Resdal Dideriksen,et al.Long-term outcomes in young patients with atrioventricular block of unknown aetiology.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab060
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#房室传导阻滞#
84
#传导阻滞#
66
学习
97
#ART#
52
#长期结局#
71
#年轻患者#
69
#HEART#
59
重视
109