Eur Urol:铂治疗的局部晚期或转移性尿路上皮癌患者的Atezolizumab与化疗治疗比较
2021-05-09 AlexYang MedSci原创
Atezolizumab是一种抗PD-L1免疫检查点抑制剂,推荐用于治疗先前含铂化疗后的局部晚期或转移性尿路上皮癌(mUC)。
Atezolizumab是一种抗PD-L1免疫检查点抑制剂,推荐用于治疗先前含铂化疗后的局部晚期或转移性尿路上皮癌(mUC)。

最近,有研究人员对IMvigor211意向性治疗(ITT)人群的总生存(OS)和安全性进行了长期随访的探索性分析。
基于铂的化疗期间或之后,研究人员将患有mUC和疾病进展的患者按1:1的比例随机接受atzolizumab 1200mg治疗或化疗(根据研究者的选择:vinflunine 320mg/m2, paclitaxel 175mg/m2 或docetaxel 75mg/m2),每3周静脉注射。尽管主要分析没有显示接受atzolizumab与化疗的患者相比有统计学意义上显著的更长的OS,但更新的OS显示了长期持久的缓解。研究结果发现,在中位数为33个月的随访中,atzolizumab治疗的24个月OS率为23%,化疗为13%。安全性研究结果与主要分析一致,没有发现新的信息。化疗患者经历了更多的3/4级治疗相关不良事件(AEs;43% vs 22%)和更多导致治疗中止的AEs(18% vs 9%)。Atezolizumab治疗的患者经历了更多特别关注的AE(35% vs 20%),这些AE往往是1-2级。
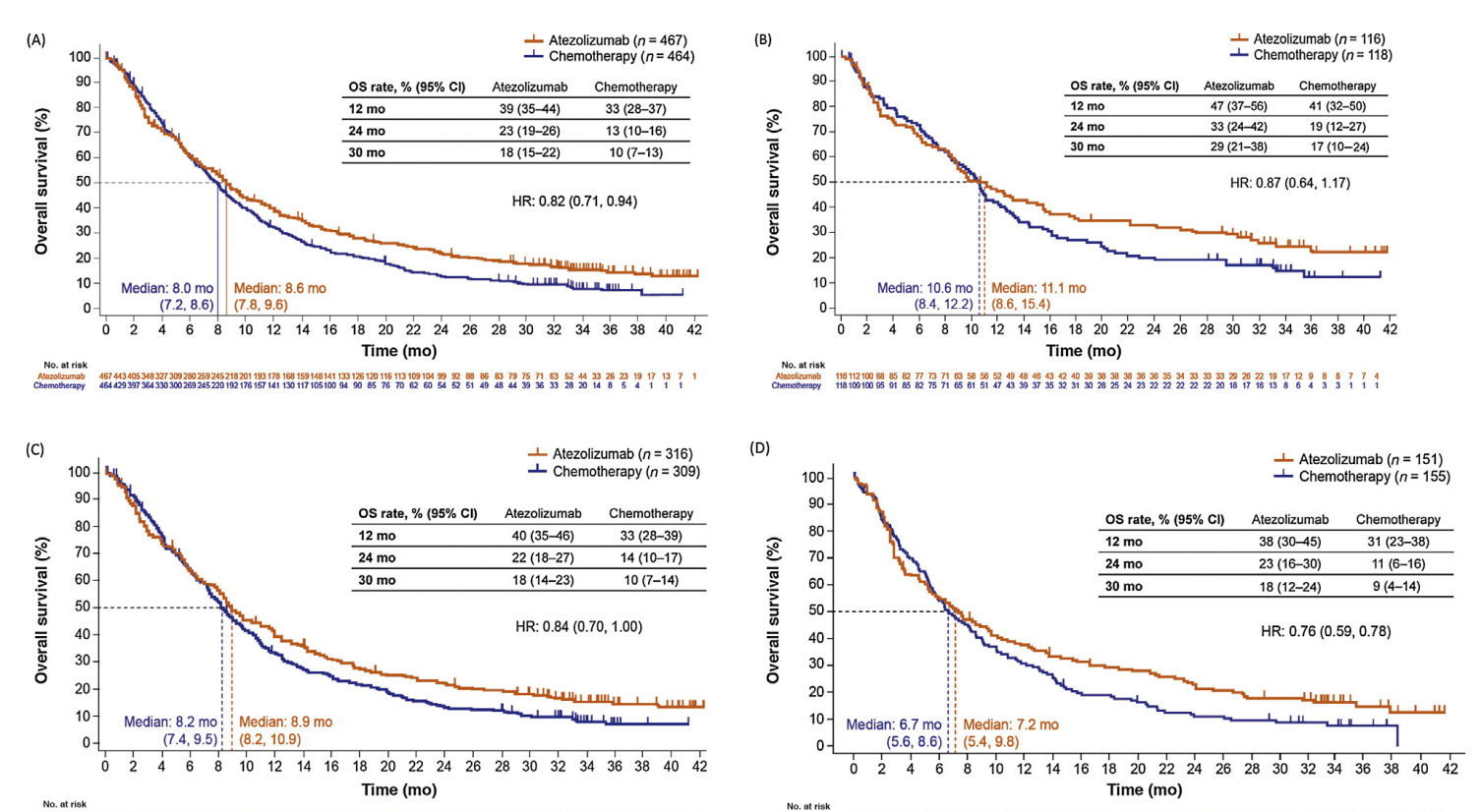
最后,研究人员指出,他们的研究结果支持了在铂类治疗mUC患者中使用atezolizumab,而不考虑PD-L1状态。他们报告了一项对已经接受过含铂化疗的膀胱癌患者进行免疫治疗(atezolizumab)的后续研究结果。他们的分析比较了开始治疗后2.5年内atezolizumab与化疗的效果。结果显示,与接受化疗的患者相比,接受atezolizumab的患者寿命更长,而且副作用可控。
原始出处:
Michiel S van der Heijden, Yohann Loriot, Ignacio Durán et al. Atezolizumab Versus Chemotherapy in Patients with Platinum-treated Locally Advanced or Metastatic Urothelial Carcinoma: A Long-term Overall Survival and Safety Update from the Phase 3 IMvigor211 Clinical Trial. Eur Urol. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#局部晚期或转移性尿路上皮癌#
66
#铂#
69
#mAb#
73
#局部晚期#
59
#转移性#
68
#转移性尿路上皮癌#
97
#局部#
67
#上皮癌#
78
#治疗比较#
92