快!病人大咯血了
2016-12-20 李沐梓 医学界呼吸频道
一例病例患者:男,55岁,已婚。20余年前诊断为“肺结核、结核性胸膜炎”,给予抗痨治疗2个月停药,未复查。2016年5月25日患者无明显诱因咯出鲜红色血液约50ml,就诊于当地医院,胸部 CT示:双肺陈旧性结核,给予止血治疗无好转,每日咯血约50ml,于2016年6月26日上午咯血约150ml,偶有咳嗽,无发热、盗汗、胸闷、胸痛及呼吸困难,为求进一步治疗,隧以“肺结核大咯血”收住入院。当遇到这样的
患者:男,55岁,已婚。
20余年前诊断为“肺结核、结核性胸膜炎”,给予抗痨治疗2个月停药,未复查。2016年5月25日患者无明显诱因咯出鲜红色血液约50ml,就诊于当地医院,胸部 CT示:双肺陈旧性结核,给予止血治疗无好转,每日咯血约50ml,于2016年6月26日上午咯血约150ml,偶有咳嗽,无发热、盗汗、胸闷、胸痛及呼吸困难,为求进一步治疗,隧以“肺结核大咯血”收住入院。
当遇到这样的一例大咯血患者,你首先会怎么处理?(给您1分钟思考。)
来看各项辅助检查结果及诊治过程......
体格检查:体温:37.3℃,脉搏:80次/分,呼吸:20次/分,血压:120/70mm Hg。胸廓对称无畸形,胸骨无压痛,触诊语颤正常两侧对称,未触及胸膜摩擦感。双肺叩诊呈清音,两肺呼吸音清,未闻及干湿性啰音。心,80次/分,律齐,各瓣膜听诊区未闻及杂音。
辅助检查:血沉10mm/h、红细胞4.15×1012/L、血红蛋白 115g/L、血小板 238×109/L、白细胞7.24×109/L、中性粒细胞百分比72.3%、淋巴细胞百分比 18.6%、单核细胞百分比4.3%,CT 示:双肺上叶可见多个结节样及条索状密度增高影,病灶边界清并钙化。双上肺及胸膜下见广泛透亮度增高影,壁薄,边界清晰。纵隔间隙可见数个钙化淋巴结影,床旁心电图示:左束支不完全性传导阻滞。
诊断:双肺继发结核并大咯血
治疗:入院后给予鼻导管氧气吸入,氨甲环酸、白眉蛇毒血凝酶、脑垂体后叶素止血治疗,效果差。介入止血治疗提示:支气管动脉造影顺利,未见支气管动脉出血;气管镜检查见:右下叶后基地段出血点,未见明显肿物;活检病理:“右下叶后基底段”少许炎性纤维素性坏死组织,抗酸(-);肺血管重建提示:双侧肺动脉栓塞。给予低分子肝素钠 5000 单位皮下注射 q12h,华法林5 mg 口服qd,定期复查凝血,根据结果而进行抗凝剂量调整治疗,患者临床症状好转后出院。
大咯血是呼吸科常见的严重急症,如何及时的正确规范处理咯血关系到患者的生命安全及医生的职业规范。
所谓咯血,指的是喉及喉以下的呼吸道(喉腔、气管、支气管和肺组织)出血且经咳嗽动作由口腔咯出。咯血不是具体的疾病,而是一组临床综合征,是一种疾病或几种疾病共同作用的结果。
咯血或痰中带血是呼吸内科常见的临床症状,引起咯血的病因复杂,几乎涉及全身各个系统,故常易误诊[1]。有文献报道,引起咯血的疾病至少有100余种以上,其中主要是呼吸系统疾病[2],90%的咯血归因于支气管扩张症、肺结核和肺脓肿[3]。
临床上由于各种原因仍然有部分患者往往因为不能及时明确诊断而未得到有效的治疗,且该病往往病情凶险,病死率高,因此早期明确诊断,及时与口腔、鼻、咽部出血或上消化道出血引起的呕血等疾病相鉴别,有助于降低病死率和改善预后[4]。
咯血与口腔、鼻、咽部出血的鉴别,应如何准确抓住各类疾病的特点?

因此,在临床上必须仔细询问病史,认真检查,包括胸部 X 线片、肺 CT、纤维支气管镜、结核菌素试验、细胞学检查及痰培养等。
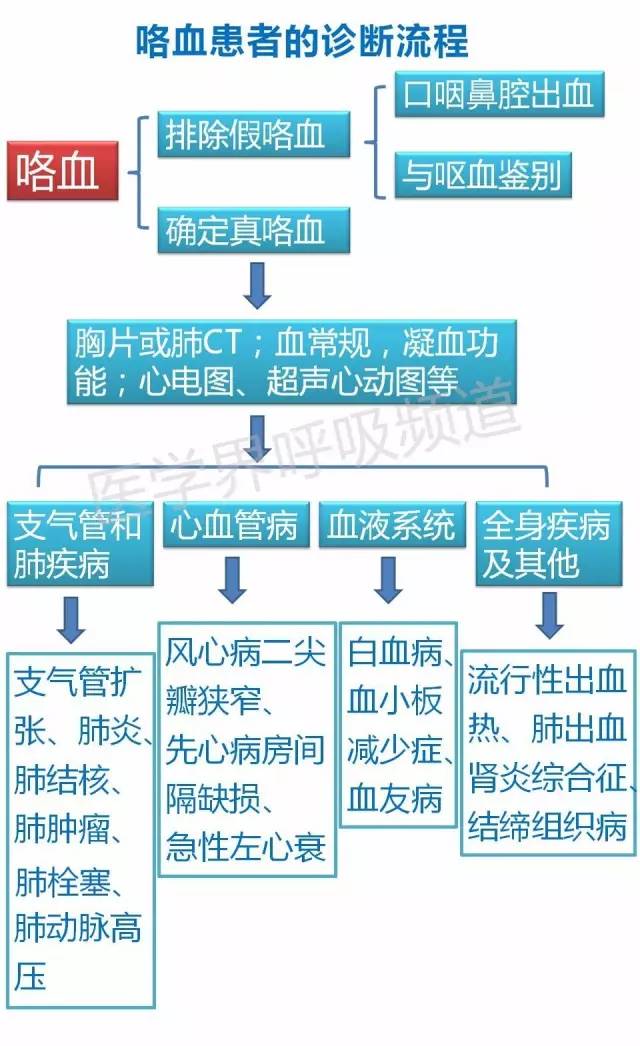
前面提到,咯血并不是具体的疾病,而是一组临床综合征,是一种疾病或几种疾病共同作用的结果。那么,在排除假性咯血后,如何找出出血的诱因加以治疗?
咯血的治疗原则包括:制止出血,治疗原发病,防止并发症,维持患者生命功能。
镇静、休息等一般措施
肺炎患者偶尔也会有咯血,多以血痰的形式发生,即使是肺结核、支气管扩张症等常见咯血疾病,也可能仅仅是小量咯血,轻微的咯血无需紧张,无需特殊处理,但要警惕有发生大咯血可能(尤其是肺结核、支气管扩张症患者)。中量以上咯血需要卧床休息,保持心情平静很重要,如果患者精神过度紧张、恐惧不安等,可给予少量镇静药,比如安定10mg口服或肌肉注射。如患者伴有剧烈咳嗽(这可能导致大咯血),应适当止咳。同时准备好静脉通道,跟家属交代好病情,言明有大咯血可能。
密切观察
这个举措非常重要,它能让我们及早反应。如果是中量以上咯血,应给予心电监护,密切观察心率、血压变化。保持呼吸道通畅,床边放置负压吸痰器,随时准备吸痰。保持大便通畅,除了嘱咐患者多喝水外,可以适当使用通便药物(比如乳果糖口服液、聚乙二醇4000散等),患者便秘时的憋气使劲很容易酿出大祸。
止血药的使用
最经典有用的药物是垂体后叶素,该药能收缩肺小动脉,使局部血流减少、血栓形成而止血。可将5-10U神经垂体素溶于20-40 ml葡萄糖溶液中缓慢静脉注射,然后10-20U神经垂体素溶于250-500 ml液体中静滴,滴速0.1 U/kg/h。很多资料显示垂体后叶素禁用于高血压、冠心病、心力衰竭等患者,因为该药可导致血压升高,恐有意外,但也有人认为可同时用硝酸甘油,而且临床很多人报道其实禁忌症并非总是禁忌症,酌情选择。另外一个常用药物是酚妥拉明,一种α肾上腺素受体阻断剂,可直接扩张血管平滑肌,降低肺动静脉压而止血,10-20 mg本药加入5%葡萄糖溶液500ml中静滴。也有报道可将上述两者联用,二者互补长短。
至于6-氨基己酸、酚磺乙胺、卡巴克洛等止血药的止血疗效不是很确切,用于小量咯血或许可以,但企图靠它们对付中、大量咯血是不靠谱的。此外还有维生素K、纤维蛋白原、云南白药等。
介入止血
经过药物治疗无效的咯血,可以考虑用气管镜止血,或者气管镜下冷盐水灌洗(4°C冷盐水500 ml加肾上腺素5 mg,分次注入出血肺段,保留1分钟后吸出),或激光冷冻止血。此外,大咯血患者还可以考虑支气管动脉栓塞术或外科手术治疗。
大咯血窒息的处理
首先判断患者是大咯血窒息。冷静果断处理!保持患者呼吸道通畅,足高头低位,拍背,想办法清除口腔及咽喉部积血(包括气管插管或切开)。
参考资料:
[1]顾钰,杜洁红,王芙蕊.老年人咯血204例原因分析[J].中国综合临床杂志,2009,23( 13) : 30.
[2]李强.呼吸病介入诊断学[M].北京: 人民军医出版社,2003:234.
[3]Cahill BC,Ingbar DH.Massive hemoptysis.Assessment and man-agement[J].Clin Chest Med,1994,15( 1) : 147-167.
[4]冯书钦.咯血300例病因分析[J].中国基层医药杂志,2008,15( 9) : 1539.
[5]中华医学会。临床诊疗指南呼吸病学分册
[6]临床药物治疗学(呼吸性疾病)。第八版
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#大咯血#
66
大咯血,是相当凶险的
97
#咯血#
83
好恐怖
74
分类清晰有理
97
学习了,谢谢!
76
学习了。。。。。
0
有用。。。。
0
学习了,很详细!谢谢
35
肺结核大咯血用垂体后叶素收缩血管止血
34