抗癌免疫疗法新药获成功
2016-09-12 佚名 生物谷
(图片摘自www.sciencealert.com)科学家们最近研究出了一种能够有效杀伤恶性胰腺癌的药物,而且没有伴随明显的副作用。 该药物叫做“IMM-101”,它能够唤醒体内的免疫系统从而对肿瘤进行杀伤。由于胰腺癌自然状态下会主动逃避体内免疫系统的识别,因此该药物的出现对于该类肿瘤的治疗具有重大的意义。 来自英国伦敦大学的研究者们通过将IMM-101与已有的化疗药物gemcitab

(图片摘自www.sciencealert.com)
科学家们最近研究出了一种能够有效杀伤恶性胰腺癌的药物,而且没有伴随明显的副作用。
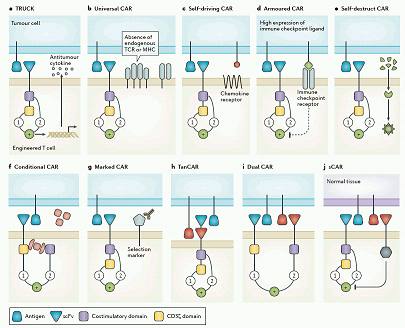
该药物叫做“IMM-101”,它能够唤醒体内的免疫系统从而对肿瘤进行杀伤。由于胰腺癌自然状态下会主动逃避体内免疫系统的识别,因此该药物的出现对于该类肿瘤的治疗具有重大的意义。
来自英国伦敦大学的研究者们通过将IMM-101与已有的化疗药物gemcitabine进行联合使用,发现其能够有效杀伤胰腺癌细胞外周的保护性细胞,以及能够延长转移胰腺癌患者的寿命。
“这对我来说是十分兴奋的”,首席研究者Angus Dalgleish说道。“这是我们首次找到能够帮助控制胰腺癌的免疫疗法”。
接受该免疫治疗药物的患者均表示相比传统化学疗法要舒服一些。而且研究结果表明该疗法没有明显的副作用。
虽然早期的研究结果十分喜人,但这并不能说明该药物具有治愈胰腺癌的能力。而且,由于该实验仅仅囊括了110名患者,因此还需要提高样本数量来获得更加可靠的结果。
Dalgleish对于IMM-101的研究已经有很长的时间,此前也有结果表明其对皮肤癌以及肺癌有一定的治疗效果,但鉴于胰腺癌的难治现象由来已久,最近的这项研究结更加有意义。
目前研究者们计划进行下一步更大规模的研究,从而完全验证此前得到的结果。
目前晚期胰腺癌患者的寿命极短,不超过18%的患者能够坚持一年以上,而转移性的胰腺癌患者寿命更加有限。根据调查, 全球范围内的胰腺癌患者寿命仅有2.7-5.8个月。
希望IMM-101的出现能够帮助缓解这一窘境。
相关结果发表在《British Journal of Cancer》杂志上。
原始出处
Experimental drug fights cancer by 'waking up' the immune system
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了,赞一个!!!
83
学习了,赞一个!!!
68
学习了,赞一个!!!
66
继续关注
0
继续学习
122