Gastrointest Endosc.:伊索拉定可改善非甾体类抗炎药引起的小肠损伤
2014-03-05 小木lemon 丁香园
非甾体类抗炎药(NSAIDs)常被用于治疗关节炎等炎症疾病,但长期服用会引发小肠黏膜损伤,如出血、穿孔,从而导致腹膜炎发生。然而,目前除了停用NSAIDs,并未确定有效可靠的治疗方案。 为了评估马来酸伊索拉定是否可以减少因持续服用NSAIDs而引起的小肠损伤,来自日本东京大学药物研究所的Yoshihiro Isomura等做了一项研究,他们发现伊索拉定可以显著改善因长期服用非甾体类抗炎药NSAI
非甾体类抗炎药(NSAIDs)常被用于治疗关节炎等炎症疾病,但长期服用会引发小肠黏膜损伤,如出血、穿孔,从而导致腹膜炎发生。然而,目前除了停用NSAIDs,并未确定有效可靠的治疗方案。
为了评估马来酸伊索拉定是否可以减少因持续服用NSAIDs而引起的小肠损伤,来自日本东京大学药物研究所的Yoshihiro Isomura等做了一项研究,他们发现伊索拉定可以显著改善因长期服用非甾体类抗炎药NSAIDs引起的小肠损伤,其成果发表在2014年2月8日的Gastrointestinal Endoscopy杂志上。
该研究为一项前瞻性、施加干预的随机对照试验,并设置单盲法,即内镜检查医生在不知道患者的分组情况下给予诊断结果。该研究纳入的对象为经常服用常见NSAIDs至少在4周以上的患者,对他们行胶囊内镜检查是否有小肠黏膜损伤,并计算损伤的数目,其中具备任何一种小肠损伤(包括红点、黏膜中断、狭窄等)的患者为符合试验条件的受试者。
研究者对筛选后的受试者进行随机分组,分别分配到伊索拉定组(每天早晨服用4毫克)和对照组(无额外治疗药物)。该试验的主要终点是在4周的干预治疗后行第二次胶囊内镜检查时小肠粘膜损伤改善的比率。
研究中61名患者进行了第一次胶囊内镜检查,其中有41名患者有小肠损伤,占67.2%,且有21名患者存在腐蚀性或溃疡性的小肠粘膜损伤,占34.4%。而且,这种损伤率与患者是否伴随服用胃保护药无显著相关性。
在最终符合标准进行试验的41名患者中,有39名患者完成了试验全过程,伊索拉定组有19名,对照组有20名。而包含任何一种小肠粘膜损伤的改善率在伊索拉定组为84.2%,显著高于对照组45.0%,尤其腐蚀性或溃疡性的小肠粘膜损伤患者在服用伊索拉定4周后有90.9%得到了改善,而对照组为72.7%,差异有统计学意义,见下图一。
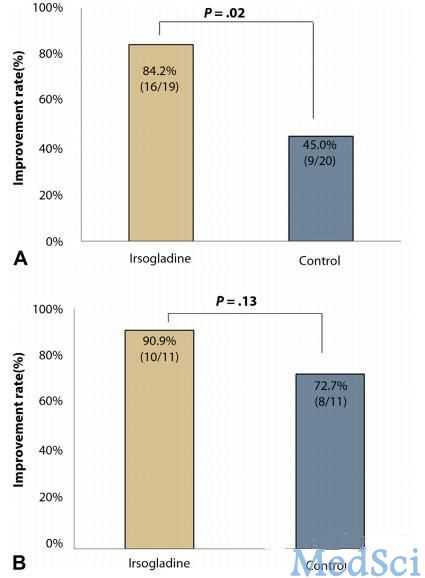
图一:A 任何一种小肠黏膜损伤的改善率;B 腐蚀性或溃疡性小肠粘膜损伤的改善率
另外,依靠受试前后两次胶囊内镜检查,研究者发现对照组小肠黏膜损伤的数目在增加(恶化)和减少(改善)上是均衡的,而伊索拉定组患者则基本是呈现损伤数目下降趋势,仅有个别患者损伤数目增加,而且即使增加,其损伤也是非常微小的(见下图二)。
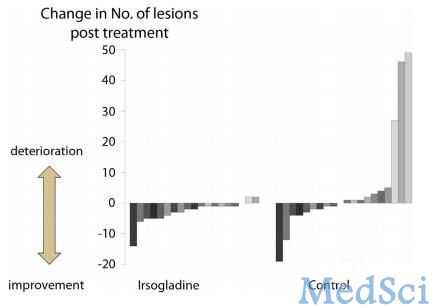
图二:胶囊内镜检查在治疗后小肠黏膜损伤数目的改变
研究表明,马来酸伊索拉定可以有效减少因持续服用NSAIDs引起的小肠损伤。但作者也提到了该研究的一定局限性,如入选患者表现为无症状的损伤,研究数据来自单中心,研究设计为单盲等。但对于目前NSAIDs药物广泛长期使用的临床背景下,其带来的副作用也困扰着越来越多的患者,该研究正是给治疗NSAIDs药物引起小肠损伤提供了一种潜在有效的方案,需要未来更深入的研究来确定有效的剂量,探索可能作用机制,并联合其他药物以优化治疗方案。
原始出处
Isomura Y, Yamaji Y, Yamada A, Watanabe Y, Suzuki H, Kobayashi Y, Yoshida S, Watabe H, Hirata Y, Yoshida H, Koike K.Irsogladine improves small-intestinal injuries in regular users of nonsteroidal anti-inflammatory drugs.Gastrointest Endosc. 2014 Feb 8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EST#
54
#AST#
75
#GAS#
56
#Test#
65
#非甾体类抗炎药#
65
#抗炎药#
63
#损伤#
63