硒化合物可让癌细胞放弃抵抗
2016-08-10 袁一雪 中国科学报
一旦癌细胞出现耐药性,任凭药物再“强横”也无计可施。所以,科学家们一边研究针对癌细胞的靶向药物,一边寻找癌细胞产生耐药性的原因,并试图阻止癌细胞这种自己保护的机制。
在全国肿瘤登记中心发布的2015年年报中显示,目前我国每年新发癌症病例约为312万例,平均每天确诊8550人,每分钟就有6人被诊断为癌症,平均10秒钟就有一人被确诊。
在目前对肿瘤治疗的方法中,化疗是一种全身性治疗,能消除原发灶及转移病灶,减少肿瘤的复发和转移。虽然化疗疗效显著,但副作用也很明显,这种药物本身毒性较高,所以限制了更高剂量的应用,也就限制了其疗效。更重要的是,肿瘤细胞对抗癌药物会产生抗药性,有数据显示,在因癌症而死亡的病人中,90%以上与肿瘤细胞的抗药性有关,尤其是多药抗药性。
一旦癌细胞出现耐药性,任凭药物再“强横”也无计可施。所以,科学家们一边研究针对癌细胞的靶向药物,一边寻找癌细胞产生耐药性的原因,并试图阻止癌细胞这种自己保护的机制。
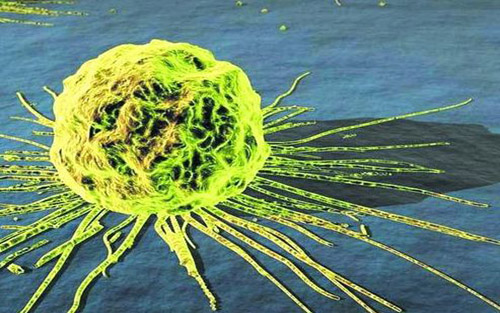
近日,来自西班牙纳瓦拉大学、波兰雅盖隆大学医学院、匈牙利塞格德大学和德国萨尔州大学的研究人员表明,一类新发现的分子,被称为硒化合物,可以杀死多耐药的小鼠癌细胞。这篇发表在《生物有机与药物化学快报》上的研究显示,这种硒化合物分子可以阻断癌细胞对抗癌药物的防御功能,从而杀灭多重耐药癌细胞。
奋起抵抗的癌细胞
这篇论文的探究结果显示,当通过化疗手段治疗癌症时,肿瘤细胞会适应这种环境并开启自我防御机制,其中包括药物外排、DNA损伤修复、生存相关基因表达上调、抗凋亡和细胞内存活信号通路激活等。其中药物外排,则是癌细胞“自带”的一种防御机制,需要“外排泵”将细胞内的药物泵出,保证癌细胞的继续存活。“不论是化疗还是靶向治疗,如果药物被癌细胞泵出,就有可能导致耐药性的产生。”中国科学院上海生命科学研究院生物化学与细胞生物学研究所研究员季红斌说(Nat Commu:肺腺癌向鳞癌转化的机制可能与YAP有关)。
这种“外排泵”,实际上是一种细胞膜上的蛋白质,被激活后可以将药物反推出细胞。而肿瘤产生耐药性的重要原因就是一种名为“ABC转运泵”在肿瘤干细胞中的过度表达。这个转运泵的家族庞大,目前发现共有49名成员,其中11个与多药抗药性有关。此次研究涉及到的就是一种名为其家族中的ABCB1。
幸运的是,此次研究还发现,这种蛋白并非会一直叛变。这篇论文的第一作者、来自西班牙纳瓦拉大学的研究人员提到,在之前的研究中,他们已经发现了57种能抑制癌细胞生长,甚至杀死癌细胞的新分子。而当翻阅关于“类似化合物”的文章后,他们发现,硒化合物可以阻断这些外排泵。
关闭癌细胞耐药通道
不仅是硒化合物,为了对抗癌细胞的耐药性,不少研究人员都投身此项研究中。
我国中山大学肿瘤防治中心实验研究部主任符立梧领衔的科研团队也一直致力于抑制肿瘤的多药抗药性的研究,并发现一系列药物可逆转或抑制肿瘤的多药抗药性。他们将原本用于植物研究领域的siRNA技术,首次用于肿瘤研究领域,发现将编码跨膜蛋白ABCB1的mdr1基因“沉默”后,可让出现抗药性的肿瘤细胞提高对抗癌药物的敏感性(中山大学肿瘤防治中心“克服ABC转运泵介导的肿瘤多药抗药性研究”获重要突破)。
2015年,来自中国科学技术大学化学与材料科学学院的梁高林课题组设计了一种可在癌细胞内“智能”自组装成纳米药物的策略,与常见的通过抑制MDR外排泵作用或利用纳米载体负载大量药物的方法不同,这些纳米药物在癌细胞内酯酶作用下缓慢释放出游离的紫杉醇从而杀死癌细胞(详细见:Nano Lett:新型评价肿瘤化疗疗效的分子成像技术现曙光)(中国科大发现克服肿瘤多药耐药新方法)。
寻找癌细胞驱动基因工程浩大
虽然针对癌细胞驱动基因的研究一直是科学家研究的重点,但是要从人体如繁星般的DNA中寻找到关键的驱动基因并予以“精准打击”着实不是件易事。“目前做得较好的是肺癌中的EGFR靶向治疗。”季红斌表示。
此次,参与研究的西班牙研究员也表示:“癌症研究的最终目的,是给予因患癌症而生命可危的人们更多机会。药物研发需要投入大量的精力和时间,而我们团队目前呈现出的结果只是初步的。但将我的努力投诸于这场战斗,即使是这些初步阶段,都使我满足。我希望,我们未来的工作能作为开发新药物的基础,到达需要它们的病人手上。”
原始出处:
Domínguez-Álvarez E, Gajdács M, Spengler G, Palop JA, Marć MA, Kieć-Kononowicz K, Amaral L, Molnár J, Jacob C, Handzlik J, Sanmartín C.Identification of selenocompounds with promising properties to reverse cancer multidrug resistance.Bioorg Med Chem Lett. 2016 Jun 15;26(12):2821-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#化合物#
64
目前做得较好的是肺癌中的EGFR靶向治疗!!!!
77
分享一下!!!
84
一旦癌细胞出现耐药性,任凭药物再“强横”也无计可施!!!
85
总结的很全面!
82
幸运的是,此次研究还发现,这种蛋白并非会一直叛变!!!!
70
更重要的是,肿瘤细胞对抗癌药物会产生抗药性!!?
40
继续学习
38
继续关注
42
继续关注
50