Cardiovasc Pathol:癌症治疗相关心血管副作用
2017-08-07 王强 肿瘤资讯
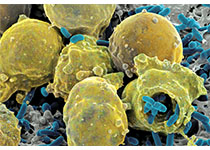
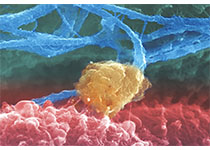
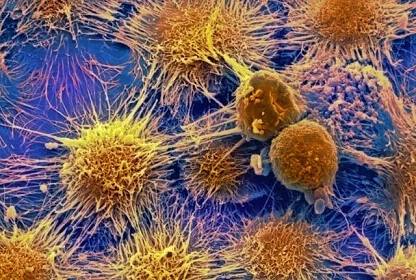
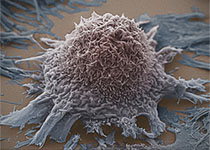
随着癌症诊疗技术的进步,带癌生存已经成为许多癌症患者的现状。因此制定肿瘤治疗方案时,除肿瘤相关预后外,还需关注治疗相关的风险及获益。本文即对癌症治疗相关心血管副作用进行概述。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ASC#
65
#副作用#
42
#Pathol#
55
#癌症治疗#
46
学习了谢谢分享!!
72
学习并分享!!
73
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
65
学习了受益匪浅
72